J Breast Cancer.
2011 Dec;14(4):314-321. 10.4048/jbc.2011.14.4.314.
Clinical Significance of Age at the Time of Diagnosis among Young Breast Cancer Patients
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. bwpark@yuhs.ac, psh1025@yuhs.ac
- 2Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2175728
- DOI: http://doi.org/10.4048/jbc.2011.14.4.314
Abstract
- PURPOSE
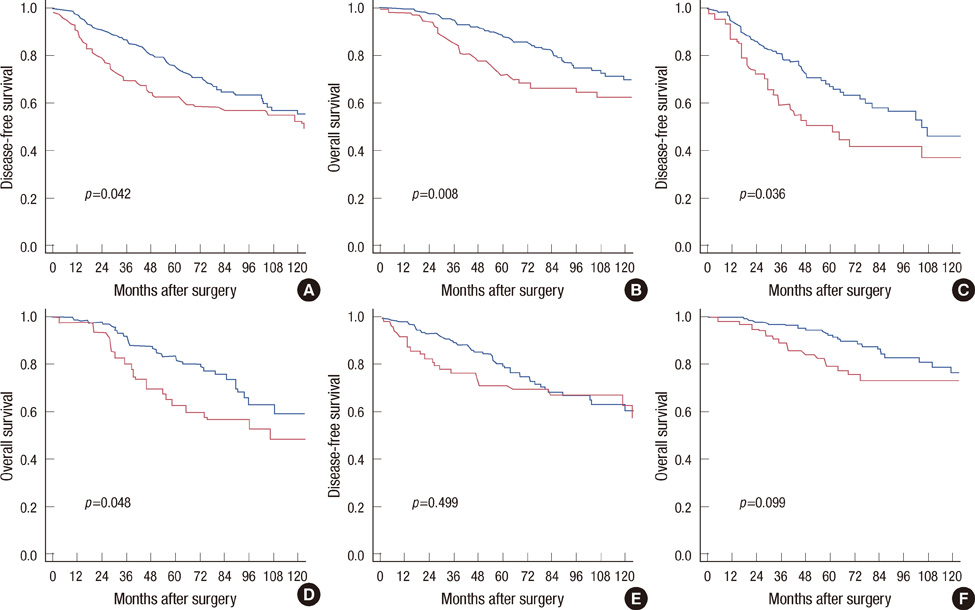
The aims of this study were to investigate outcomes corresponding to age at diagnosis as categorized into 5-year intervals and to explore whether endocrine-responsive tumors display clinical benefits from endocrine therapy after chemotherapy among young breast cancer patients.
METHODS
A total of 1,171 patients who were under 40 years old at diagnosis between 1985 and 2007 were divided into 3 subgroups: < or =30 years (Group I, 13.3%), 31-35 years (Group II, 30.5%), and 36-40 years (Control group, 56.2%). Clinicopathological factors and outcomes were compared using a chi-square test, the Kaplan-Meier method, and Cox's hazards models.
RESULTS
There were no significant differences in the characteristics and treatment patterns between the 3 groups, except for the grade, hormone receptors expression, and use of endocrine therap. Group I showed the worst survival and subsequently Group II presented worse outcomes than the Control group, mainly among hormone receptors-positive patients. Groups I and II showed increased risks of recurrence and death in multivariate analyses. Among 529 hormone receptors-positive patients who received chemotherapy, favorable outcomes for patients who were treated with endocrine agents were demonstrated, mainly in patients aged 35 years or less. However, interaction tests between the use of endocrine therapy and age at diagnosis were not significant.
CONCLUSION
Age at diagnosis is an independent prognostic factor and the age of 35 years is a rational cut-off among young patients. Our subgroup analysis suggests that endocrine therapy may provide additional benefits even in young breast cancers. Therefore, further researches should be directed towards improving outcomes for this population.
Keyword
Figure
Cited by 1 articles
-
Prognostic Impact and Clinicopathological Correlation of CD133 and ALDH1 Expression in Invasive Breast Cancer
Sung Jeep Kim, Yong Seok Kim, Eun Duok Jang, Kyung Jin Seo, Jeong Soo Kim
J Breast Cancer. 2015;18(4):347-355. doi: 10.4048/jbc.2015.18.4.347.
Reference
-
1. Elkum N, Dermime S, Ajarim D, Al-Zahrani A, Alsayed A, Tulbah A, et al. Being 40 or younger is an independent risk factor for relapse in operable breast cancer patients: the Saudi Arabia experience. BMC Cancer. 2007. 7:222.
Article2. Tarone RE. Breast cancer trends among young women in the United States. Epidemiology. 2006. 17:588–590.
Article3. Shin HR, Jung KW, Won YJ, Park JG. 139 KCCR-affiliated Hospitals. 2002 annual report of the Korea Central Cancer Registry: based on registered data from 139 hospitals. Cancer Res Treat. 2004. 36:103–114.
Article4. Han W, Kim SW, Park IA, Kang D, Kim SW, Youn YK, et al. Young age: an independent risk factor for disease-free survival in women with operable breast cancer. BMC Cancer. 2004. 4:82.
Article5. Ko SS. Korean Breast Cancer Society. Chronological changing patterns of clinical characteristics of Korean breast cancer patients during 10 years (1996-2006) using nationwide breast cancer registration on-line program: biannual update. J Surg Oncol. 2008. 98:318–323.
Article6. Han W, Kang SY. Korean Breast Cancer Society. Relationship between age at diagnosis and outcome of premenopausal breast cancer: age less than 35 years is a reasonable cut-off for defining young age-onset breast cancer. Breast Cancer Res Treat. 2010. 119:193–200.
Article7. Kim EK, Noh WC, Han W, Noh DY. Prognostic significance of young age (<35 years) by subtype based on ER, PR, and HER2 status in breast cancer: a nationwide registry-based study. World J Surg. 2011. 35:1244–1253.
Article8. Goldhirsch A, Glick JH, Gelber RD, Coates AS, Thürlimann B, Senn HJ, et al. Meeting highlights: international expert consensus on the primary therapy of early breast cancer 2005. Ann Oncol. 2005. 16:1569–1583.
Article9. Aebi S, Gelber S, Castiglione-Gertsch M, Gelber RD, Collins J, Thürlimann B, et al. Is chemotherapy alone adequate for young women with oestrogen-receptor-positive breast cancer? Lancet. 2000. 355:1869–1874.
Article10. Goldhirsch A, Gelber RD, Yothers G, Gray RJ, Green S, Bryant J, et al. Adjuvant therapy for very young women with breast cancer: need for tailored treatments. J Natl Cancer Inst Monogr. 2001. (30):44–51.
Article11. Jung M, Shin HJ, Rha SY, Jeung HC, Hong S, Moon YW, et al. The clinical outcome of chemotherapy-induced amenorrhea in premenopausal young patients with breast cancer with long-term follow-up. Ann Surg Oncol. 2010. 17:3259–3268.
Article12. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005. 365:1687–1717.13. Ahn SH, Son BH, Kim SW, Kim SI, Jeong J, Ko SS, et al. Poor outcome of hormone receptor-positive breast cancer at very young age is due to tamoxifen resistance: nationwide survival data in Korea--a report from the Korean Breast Cancer Society. J Clin Oncol. 2007. 25:2360–2368.
Article14. Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007. 25:118–145.
Article15. Kang BM, Jung JH, Lim YS, Park HY, Lee YH. Clinical significance of age for premenopausal women with primary breast cancer. J Breast Cancer. 2006. 9:323–329.
Article16. Xiong Q, Valero V, Kau V, Kau SW, Taylor S, Smith TL, et al. Female patients with breast carcinoma age 30 years and younger have a poor prognosis: the M.D. Anderson Cancer Center experience. Cancer. 2001. 92:2523–2528.
Article17. Albain KS, Allred DC, Clark GM. Breast cancer outcome and predictors of outcome: are there age differentials? J Natl Cancer Inst Monogr. 1994. (16):35–42.18. Park BW, Kim SI, Kim EK, Yang WI, Lee KS. Impact of patient age on the outcome of primary breast carcinoma. J Surg Oncol. 2002. 80:12–18.
Article19. Weber-Mangal S, Sinn HP, Popp S, Klaes R, Emig R, Bentz M, et al. Breast cancer in young women (<or=35 years): genomic aberrations detected by comparative genomic hybridization. Int J Cancer. 2003. 107:583–592.
Article20. Kroman N, Jensen MB, Wohlfahrt J, Mouridsen HT, Andersen PK, Melbye M. Factors influencing the effect of age on prognosis in breast cancer: population based study. BMJ. 2000. 320:474–478.21. Fisher B, Dignam J, Wolmark N, DeCillis A, Emir B, Wickerham DL, et al. Tamoxifen and chemotherapy for lymph node-negative, estrogen receptor-positive breast cancer. J Natl Cancer Inst. 1997. 89:1673–1682.
Article22. Lee EH, Park SK, Park B, Kim SW, Lee MH, Ahn SH, et al. Effect of BRCA1/2 mutation on short-term and long-term breast cancer survival: a systematic review and meta-analysis. Breast Cancer Res Treat. 2010. 122:11–25.
Article23. Son BH, Ahn SH, Lee MH, Park SK, Kim SW. Korean Breast Cancer Society. Hereditary breast cancer in Korea: a review of the literature. J Breast Cancer. 2008. 11:1–9.
Article24. Han SA, Park SK, Ahn SH, Son BH, Lee MH, Choi DH, et al. The breast and ovarian cancer risks in Korea due to inherited mutations in BRCA1 and BRCA2: a preliminary report. J Breast Cancer. 2009. 12:92–99.
Article25. Koo DH, Chung IY, Kang E, Han SA, Kim SW. Usage patterns of surveillance, chemoprevention and risk-reducing surgery in Korean BRCA mutation carriers: 5 years of experience at a single institution. J Breast Cancer. 2011. 14:Suppl 1. S17–S23.26. Narod SA. BRCA mutations in the management of breast cancer: the state of the art. Nat Rev Clin Oncol. 2010. 7:702–707.
Article27. Hickey M, Peate M, Saunders CM, Friedlander M. Breast cancer in young women and its impact on reproductive function. Hum Reprod Update. 2009. 15:323–339.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unique Features of Young Age Breast Cancer and Its Management
- Study of the Survival of Women Aged 35 and Younger with Breast Cancer
- Prognosis of Breast Cancer Occurring in Patients below the Age of 35 Years Compared with Groups above the Age of 36 Years
- The Clinical Significance and Prognosis of Korean Young Age (younger or 35 year old) onset Breast Cancer
- Clinicopathological Characteristics and Prognosis of Breast Cancer in Young Women Under 35 Years of Age