Intest Res.
2016 Jan;14(1):83-88. 10.5217/ir.2016.14.1.83.
Refractory pseudomembranous colitis that was treated successfully with colonoscopic fecal microbial transplantation
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Inha University School of Medicine, Incheon, Korea. bangbu@inha.ac.kr
- KMID: 2174514
- DOI: http://doi.org/10.5217/ir.2016.14.1.83
Abstract
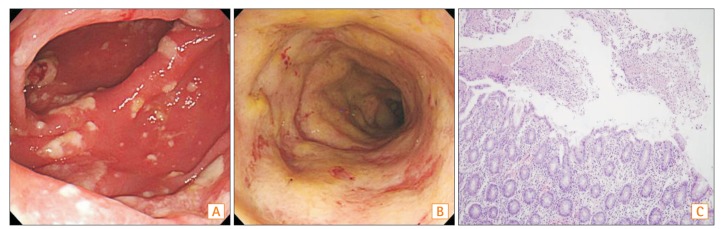
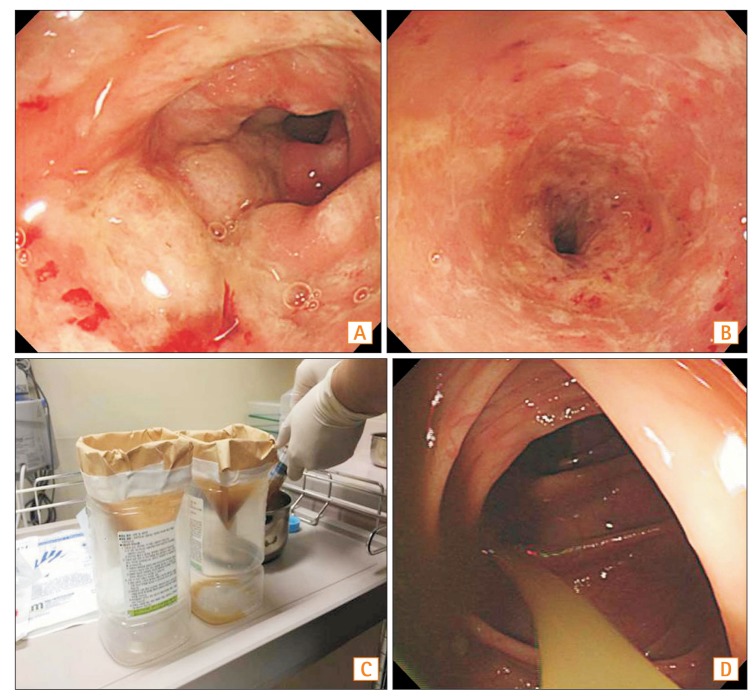
- Pseudomembranous colitis (PMC) is a nosocomial and opportunistic infection caused by Clostridium difficile. PMC is related to the use of antibiotics leading to intestinal dysbiosis and an overgrowth of C. difficile. Metronidazole or vancomycin is considered to be the standard therapy for the management of PMC. However, PMC has a 15%-30% recurrence rate and can be refractory to standard treatments, resulting in morbidity and mortality. Here we describe a patient who experienced refractory PMC who was treated with fecal microbiota transplantation. A 69-year-old woman was admitted to the hospital with consistent abdominal pain and diarrhea, which had been present for 5 months. She was diagnosed with PMC by colonoscopy and tested positive for C. difficile toxin. Even though she took metronidazole for 10 days, followed by vancomycin for 4 weeks, her symptoms did not improve. Because of her recurrent and refractory symptoms, we decided to perform fecal microbiota transplantation. Fifty grams of fresh feces from a donor were obtained on the day of the procedure, mixed with 500 mL of normal saline, and then filtered. The filtered solution was administered to the patient's colon using a colonoscope. After the procedure, her symptoms rapidly improved and a follow-up colonoscopy showed that the PMC had resolved without recurrence.
Keyword
MeSH Terms
-
Abdominal Pain
Aged
Anti-Bacterial Agents
Clostridium difficile
Colon
Colonoscopes
Colonoscopy
Diarrhea
Dysbiosis
Enterocolitis, Pseudomembranous*
Feces
Female
Follow-Up Studies
Humans
Metronidazole
Microbiota
Mortality
Opportunistic Infections
Recurrence
Tissue Donors
Vancomycin
Anti-Bacterial Agents
Metronidazole
Vancomycin
Figure
Cited by 1 articles
-
Fecal Microbiota Transplantation for Refractory and Recurrent Clostridium difficile Infection: A Case Series of Nine Patients
Byoung Wook Bang, Jin-Seok Park, Hyung Kil Kim, Yong Woon Shin, Kye Sook Kwon, Hea Yoon Kwon, Ji Hyeon Baek, Jin-Soo Lee
Korean J Gastroenterol. 2017;69(4):226-231. doi: 10.4166/kjg.2017.69.4.226.
Reference
-
1. Kelly CP, LaMont JT. Clostridium difficile — more difficult than ever. N Engl J Med. 2008; 359:1932–1940.2. Lee YJ, Choi MG, Lim CH, et al. Change of Clostridium difficile colitis during recent 10 years in Korea. Korean J Gastroenterol. 2010; 55:169–174. PMID: 20357527.
Article3. Lee JH, Lee SY, Kim YS, et al. The incidence and clinical features of Clostridium difficile infection; single center study. Korean J Gastroenterol. 2010; 55:175–182. PMID: 20357528.
Article4. Seo GS. Clostridium difficile Infection: What's New? Intest Res. 2013; 11:1–13.5. Wilcox MH. Descriptive study of intravenous immunoglobulin for the treatment of recurrent Clostridium difficile diarrhoea. J Antimicrob Chemother. 2004; 53:882–884. PMID: 15073160.
Article6. Kelly CP. Fecal microbiota transplantation — an old therapy comes of age. N Engl J Med. 2013; 368:474–475. PMID: 23323865.
Article7. Pepin J. Improving the treatment of Clostridium difficile-associated disease: where should we start? Clin Infect Dis. 2006; 43:553–555. PMID: 16886145.
Article8. van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013; 368:407–415. PMID: 23323867.
Article9. Eiseman B, Silen W, Bascom GS, Kauvar AJ. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery. 1958; 44:854–859. PMID: 13592638.10. Kelly CR, de Leon L, Jasutkar N. Fecal microbiota transplantation for relapsing Clostridium difficile infection in 26 patients: methodology and results. J Clin Gastroenterol. 2012; 46:145–149. PMID: 22157239.11. Moon KR, Sohn KM, Park BM, et al. Successful fecal transplantation by enema for recurrent and refractory Clostridium difficile infection. J Korean Geriatr Soc. 2013; 17:152–156.12. Gweon TG, Choi MG, Lee SK, et al. Two cases of refractory pseudomembranous colitis that healed following fecal microbiota transplantation. Korean J Med. 2013; 84:395–399.13. Burke KE, Lamont JT. Fecal transplantation for recurrent Clostridium difficile infection in older adults: a review. J Am Geriatr Soc. 2013; 61:1394–1398. PMID: 23869970.14. Yoon SS, Brandt LJ. Treatment of refractory/recurrent C. difficile-associated disease by donated stool transplanted via colonoscopy: a case series of 12 patients. J Clin Gastroenterol. 2010; 44:562–566. PMID: 20463588.15. Gough E, Shaikh H, Manges AR. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis. 2011; 53:994–1002. PMID: 22002980.16. Cohen SH, Gerding DN, Johnson S, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431–455. PMID: 20307191.
Article17. Bauer MP, Kuijper EJ, van Dissel JT. European Society of Clinical Microbiology and Infectious Diseases. European Society of Clinical Microbiology and Infectious Diseases (ESCMID): treatment guidance document for Clostridium difficile infection (CDI). Clin Microbiol Infect. 2009; 15:1067–1079. PMID: 19929973.
Article18. Fekety R, Silva J, Kauffman C, Buggy B, Deery HG. Treatment of antibiotic-associated Clostridium difficile colitis with oral vancomycin: comparison of two dosage regimens. Am J Med. 1989; 86:15–19. PMID: 2910090.
Article19. Rohlke F, Stollman N. Fecal microbiota transplantation in relapsing Clostridium difficile infection. Therap Adv Gastroenterol. 2012; 5:403–420.
Article20. Kang J. Fecal Bacteriotherapy for Recurrent Clostridium difficile infection: a systemic literature review. Korean J Nosocomial Infect Control. 2012; 17:70–78.21. Youngster I, Russell GH, Pindar C, Ziv-Baran T, Sauk J, Hohmann EL. Oral, capsulized, frozen fecal microbiota transplantation for relapsing Clostridium difficile infection. JAMA. 2014; 312:1772–1778. PMID: 25322359.
Article22. Lee CH, Belanger JE, Kassam Z, et al. The outcome and longterm follow-up of 94 patients with recurrent and refractory Clostridium difficile infection using single to multiple fecal microbiota transplantation via retention enema. Eur J Clin Microbiol Infect Dis. 2014; 33:1425–1428. PMID: 24627239.
Article23. Brandt LJ, Aroniadis OC, Mellow M, et al. Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection. Am J Gastroenterol. 2012; 107:1079–1087. PMID: 22450732.
Article24. Debast SB, Bauer MP, Kuijper EJ. European Society of Clinical Microbiology and Infectious Diseases. European Society of Clinical Microbiology and Infectious Diseases: update of the treatment guidance document for Clostridium difficile infection. Clin Microbiol Infect. 2014; 20(Suppl 2):1–26. PMID: 24118601.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Refractory Pseudomembranous Colitis that Healed Following Fecal Microbiota Transplantation
- Ischemic colitis complicated by Clostridioides difficile infection treated with fecal microbiota transplantation
- Refractory Clostridium difficile Infection Cured With Fecal Microbiota Transplantation in Vancomycin-Resistant Enterococcus Colonized Patient
- A case of amebic colitis mimicking pseudomembranous colitis
- A Case of Toxic Megacolon Caused by Clostridium difficile Infection and Treated with Fecal Microbiota Transplantation