J Gynecol Oncol.
2011 Dec;22(4):269-274. 10.3802/jgo.2011.22.4.269.
Prediction of a high-risk group based on postoperative nadir CA-125 levels in patients with advanced epithelial ovarian cancer
- Affiliations
-
- 1Branch of Uterine Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea. sokbom@ncc.re.kr
- 2Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2173629
- DOI: http://doi.org/10.3802/jgo.2011.22.4.269
Abstract
OBJECTIVE
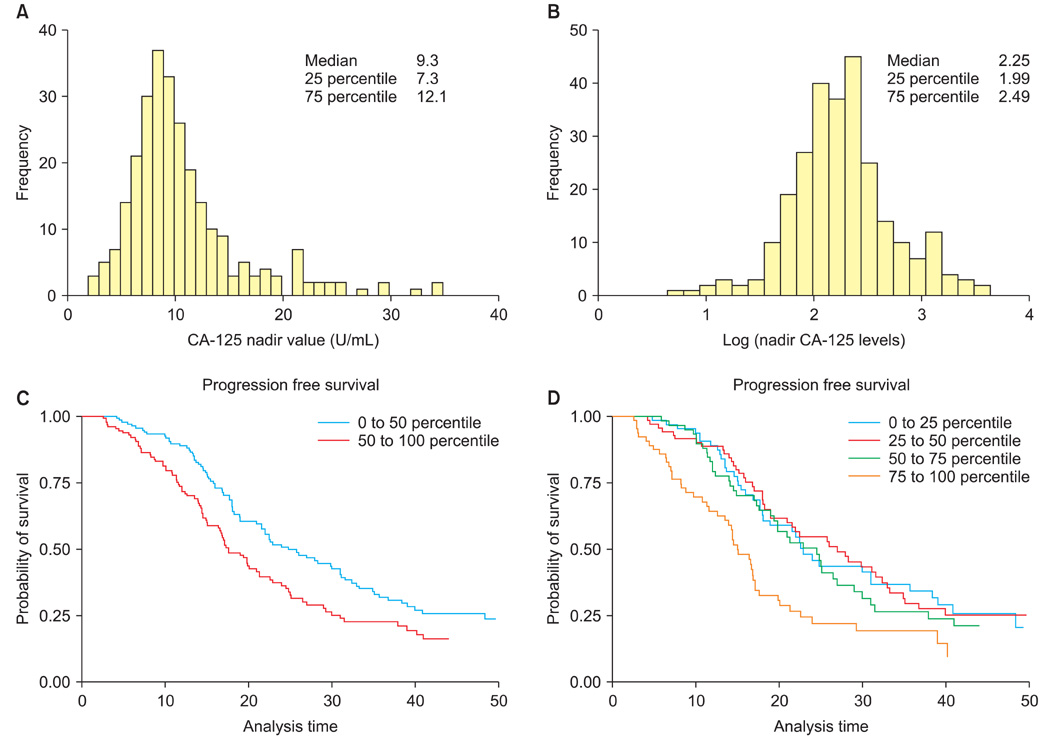
We aimed to determine the ideal cut-off of nadir serum CA-125 level for prediction of progression free survival.
METHODS
Among 267 patients who achieved complete remission after chemotherapy, the correlation between nadir CA-125 and progression free survival were compared among the subgroups classified according to the distribution of CA-125. The diagnostic odds ratio and area under the receiver operator characteristics curve were compared at various cut-off points.
RESULTS
The nadir CA-125 levels did not have prognostic value under 12 U/mL (to 75 percentile). In contrast, they were significantly correlated with progression free survival only when the CA-125 level was greater than 12, which was 75 percentile (p=0.034). In predicting progression free survival <6 and 12 months, the cut-off value of 18 (90 percentile) showed superior diagnostic performance over 10 or 12 U/mL. Compared with patients who showed nadir levels between 0 and 12 U/mL (0 to 75 percentile), those with nadir >18 U/mL showed a hazard ratio of 2.85 (95% confidence interval, 1.70 to 4.76; p<0.001); patients with nadir levels between 18 and 12 U/mL showed a the hazard ratio of 1.68 (95% confidence interval, 1.11 to 2.56; p=0.015) compared with those whose nadir levels were under 12 U/mL.
CONCLUSION
The predictive power of the traditional cut-off of 10 U/mL to classify a risk group or to identify high risk patients was unsatisfactory. The optimal diagnostic performance was observed at the cut-off of 18 U/mL and this can be proposed to dichotomize cut-off values to predict outcomes among individual patients.
MeSH Terms
Figure
Reference
-
1. Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, et al. Cancer statistics, 2005. CA Cancer J Clin. 2005. 55:10–30.2. Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol. 2003. 21:3194–3200.3. Armstrong DK, Brady MF. Intraperitoneal therapy for ovarian cancer: a treatment ready for prime time. J Clin Oncol. 2006. 24:4531–4533.4. Olt GJ, Berchuck A, Bast RC Jr. Gynecologic tumor markers. Semin Surg Oncol. 1990. 6:305–313.5. Skates SJ, Horick NK, Moy JM, Minihan AM, Seiden MV, Marks JR, et al. Pooling of case specimens to create standard serum sets for screening cancer biomarkers. Cancer Epidemiol Biomarkers Prev. 2007. 16:334–341.6. Makar AP, Kristensen GB, Kaern J, Bormer OP, Abeler VM, Trope CG. Prognostic value of pre- and postoperative serum CA 125 levels in ovarian cancer: new aspects and multivariate analysis. Obstet Gynecol. 1992. 79:1002–1010.7. Crawford SM, Peace J. Does the nadir CA-125 concentration predict a long-term outcome after chemotherapy for carcinoma of the ovary? Ann Oncol. 2005. 16:47–50.8. Juretzka MM, Barakat RR, Chi DS, Iasonos A, Dupont J, Abu-Rustum NR, et al. CA-125 level as a predictor of progression-free survival and overall survival in ovarian cancer patients with surgically defined disease status prior to the initiation of intraperitoneal consolidation therapy. Gynecol Oncol. 2007. 104:176–180.9. Markman M, Liu PY, Rothenberg ML, Monk BJ, Brady M, Alberts DS. Pretreatment CA-125 and risk of relapse in advanced ovarian cancer. J Clin Oncol. 2006. 24:1454–1458.10. Prat A, Parera M, Peralta S, Perez-Benavente MA, Garcia A, Gil-Moreno A, et al. Nadir CA-125 concentration in the normal range as an independent prognostic factor for optimally treated advanced epithelial ovarian cancer. Ann Oncol. 2008. 19:327–331.11. Kang S, Seo SS, Park SY. Nadir CA-125 level is an independent prognostic factor in advanced epithelial ovarian cancer. J Surg Oncol. 2009. 100:244–247.12. Pignata S, Perrone F, Di Maio M, Gallo C, De Placido S. In Reply. J Clin Oncol. 2005. 23:2436–2437.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic value of serum CA-125 in patients with advanced epithelial ovarian cancer followed by complete remission after adjuvant chemotherapy
- Prediction of Size of Residual Discase after Initial Surgery by Postoperative Decline of Serum CA 125 Levels in Patients with Advanced Epithelial Ovarian Cancer
- The Prognostic Significance of Serum CA 125 Levels in Patients with Advanced Serous Epithelial Ovarian Cancer
- The clinical value of serum TPS and CA 125 in the diagnosis of epithelial ovarian cancer
- An Immunohistochemical Study of CA 125, CA 19-9, and CA 15-3 in Ovarian Epithelial Tumors