Ewha Med J.
2015 Oct;38(3):106-111. 10.12771/emj.2015.38.3.106.
Clinical Features and Response to UDCA Treatment of Primary Biliary Cirrhosis
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea. thkm@ewha.ac.kr
- 2Department of Pathology, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2171346
- DOI: http://doi.org/10.12771/emj.2015.38.3.106
Abstract
OBJECTIVES
Primary biliary cirrhosis (PBC) is a chronic cholestatic liver disease that may progress to end stage liver cirrhosis. Benefits of ursodeoxycholic acid (UDCA) treatment has been investigated through large clinical studies. However, most of the studies were done in western countries and recent increase in prevalence of this relatively uncommon chronic liver disease draws attention in Korea. As early UDCA treatment effectively prevent the grave consequences of PBC progression, early diagnosis and lifelong management with UDCA is important. This study was designed to investigate the clinical features of PBC and response rates of UDCA treatments in Ewha Womans University Medical Center.
METHODS
Clinical data of PBC patients diagnosed between 2001 and 2014 at Ewha Womans University Medical Center were analyzed retrospectively.
RESULTS
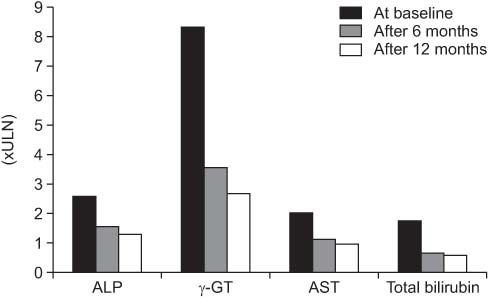
A total of 35 patients with mean follow-up duration of 42 months were enrolled. At the diagnosis, 72.7% of the patients were asymptomatic, 5.7% had decompensated liver cirrhosis. The mean serum alkaline phosphate (ALP) level was 2.65 times upper limit of normal. UDCA was prescribed in 91.4% of the patients (n=32), among which 77.4% exhibited biochemical responses defined as serum ALP less than 2 upper limit of normal at 6 months (Mayo criteria).
CONCLUSION
Most PBC patients were asymptomatic at the time of diagnosis and the average biochemical responses rate to UDCA treatment were ranged from 60.0% to 78.9% according to various response criteria. To elucidate the clinical features and courses of Korean PBC patients in detail, larger scale investigations and longer clinical follow up studies are warranted.
Keyword
MeSH Terms
Figure
Reference
-
1. Kaplan MM, Gershwin ME. Primary biliary cirrhosis. N Eng J Med. 2005; 353:1261–1273.2. Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ. Primary biliary cirrhosis. Hepatology. 2009; 50:291–308.3. Metcalf J, James O. The geoepidemiology of primary biliary cirrhosis. Semin Liver dis. 1997; 17(1):13–22.4. Chon C. Primary biliary cirrhosis-multicenter study. Korean J Hepatol. 2004; 10:s3–s4.5. Kim KA, Jeong SH, Lee JI, Yeon JE, Lee HJ, Kwon SY, et al. Clinical features and prognosis of primary biliary cirrhosis in Korea. Korean J Hepatol. 2010; 16:139–146.6. Kim WR, Wiesner RH, Poterucha JJ, Therneau TM, Benson JT, Krom RA, et al. Adaptation of the Mayo primary biliary cirrhosis natural history model for application in liver transplant candidates. Liver Transpl. 2000; 6:489–494.7. Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001; 33:464–470.8. Ludwig J, Dickson E, McDonald GSA. Staging of chronic nonsuppurative destructive cholangitis (syndrome of primary biliary cirrhosis). Virchows Arch A Pathol Anat Histol. 1978; 379:103–112.9. Lammers WJ, Kowdley KV, van Buuren HR. Predicting outcome in primary biliary cirrhosis. Ann Hepatol. 2014; 13:316–326.10. Angulo P, Lindor KD, Therneau TM, Jorgensen RA, Malinchoc M, Kamath PS, et al. Utilization of the Mayo risk score in patients with primary biliary cirrhosis receiving ursodeoxycholic acid. Liver. 1999; 19:115–121.11. Parés A, Caballería L, Rodés J. Excellent long-term survival in patients with primary biliary cirrhosis and biochemical response to ursodeoxycholic acid. Gastroenterology. 2006; 130:715–720.12. Corpechot C, Abenavoli L, Rabahi N, Chrétien Y, Andréani T, Johanet C, et al. Biochemical response to ursodeoxycholic acid and long-term prognosis in primary biliary cirrhosis. Hepatology. 2008; 48:871–877.13. Momah N, Silveira MG, Jorgensen R, Sinakos E, Lindor KD. Optimizing biochemical markers as endpoints for clinical trials in primary biliary cirrhosis. Liver Int. 2012; 32:790–795.14. Invernizzi P, Crosignani A, Battezzati PM, Covini G, De Valle G, Larghi A, et al. Comparison of the clinical features and clinical course of antimitochondrial antibody-positive and-negative primary biliary cirrhosis. Hepatology. 1997; 25:1090–1095.15. Mendes F, Lindor KD. Antimitochondrial antibody-negative primary biliary cirrhosis. Gastroenterol Clin North Am. 2008; 37:479–484.16. Mayo MJ. Natural history of primary biliary cirrhosis. Clin Liver dis. 2008; 12:277–288.17. Metcalf JV, Mitchison HC, Palmer JM, Jones DE, Bassendine MF, James OF. Natural history of early primary biliary cirrhosis. Lancet. 1996; 348:1399–1402.18. Prince M, Chetwynd A, Newman W, Metcalf JV, James OF. Survival and symptom progression in a geographically based cohort of patients with primary biliary cirrhosis: follow-up for up to 28 years. Gastroenterology. 2002; 123:1044–1051.19. Prince M, Chetwynd A, Craig W, Metcalf J, James O. Asymptomatic primary biliary cirrhosis: clinical features, prognosis, and symptom progression in a large population based cohort. Gut. 2004; 53:865–870.20. Corpechot C, Carrat F, Bahr A, Chrétien Y, Poupon RE, Poupon R. The effect of ursodeoxycholic acid therapy on the natural course of primary biliary cirrhosis. Gastroenterology. 2005; 128:297–303.21. Park E, Lee J, Lee H, Choi Y, Koh K, Paik S. Prognosis and prognostic factors of primary biliary cirrhosis in Korea: A single center experience. Korean J Hepatol. 2006; 12:s75.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Feat uresand Response to Ursodeoxycholic Acid Therapy in Autoimmune Cholangitis and Primary Biliary Cirrhosis
- Diagnosis and Treatment of Primary Biliary Cholangitis
- Retrospective analysis of autoimmune hepatitis-primary biliary cirrhosis overlap syndrome in Korea: characteristics, treatments, and outcomes
- Liver Cirrhosis Progression in a Patient with Overlapping IgG4-Related Sclerosing Cholangitis and Primary Biliary Cholangitis
- The diagnosis and treatment of primary biliary cirrhosis