Infect Chemother.
2011 Dec;43(6):490-493. 10.3947/ic.2011.43.6.490.
A Case of Burkholderia cepacia Bacteremia and Infective Spondylitis, Treated with Ceftazidime and Trimethoprim-Sulfamethoxazole Combination Therapy, which did not Respond to Carbapenem Monotherapy
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Medical School, Gwang-ju, Korea. medkid@dreamwiz.com
- 2Department of Laboratory Medicine, Chonnam National University Medical School, Gwang-ju, Korea.
- KMID: 2170361
- DOI: http://doi.org/10.3947/ic.2011.43.6.490
Abstract
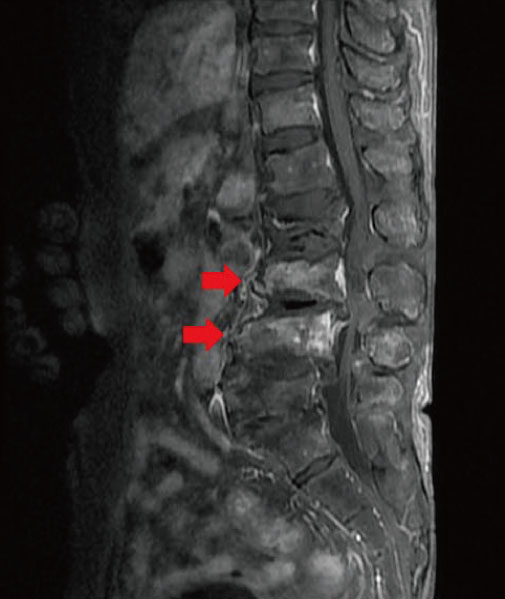
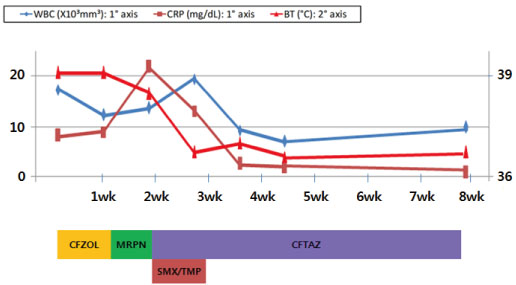
- Burkholderia cepacia is an aerobic gram-negative rod that causes healthcare-associated infections through contaminated disinfectants, fluids, and medical equipment. This bacterium shows resistance to various antibiotics. For this reason, available therapeutic antimicrobial agents are limited, and the optimal antimicrobial therapeutic regimen was still not well-determined in the case of infective spondylitis. We experienced a case of B. cepacia bacteremia with infective spondylitis and paraspinal abscesses which did not respond to carbapenem monotherapy, but was did respond to ceftazidime and sulfamethoxzaole/trimethoprim combination therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Mohr CD, Tomich M, Herfst CA. Cellular aspects of Burkholderia cepacia infection. Microbes Infect. 2001. 3:425–435.2. Speert DP. Advances in Burkholderia cepacia complex. Paediatr Respir Rev. 2002. 3:230–235.3. Marioni G, Rinaldi R, Ottaviano G, Marchese-Ragona R, Savastano M, Staffieri A. Cervical necrotizing fasciitis: a novel clinical presentation of Burkholderia cepacia infection. J Infect. 2006. 53:e219–e222.4. Held MR, Begier EM, Beardsley DS, Browne FA, Martinello RA, Baltimore RS, McDonald LC, Jensen B, Hadler JL, Dembry LM. Life-threatening sepsis caused by Burkholderia cepacia from contaminated intravenous flush solutions prepared by a compounding pharmacy in another state. Pediatrics. 2006. 118:e212–e215.5. Yang BH, Lee MS, Lee JH, Lee HJ. Pyogenic spondylitis in a healthy adult caused by Burkholderia cepacia. Infect Chemother. 2008. 40:233–236.
Article6. Smith MA, Trowers NR, Klein RS. Cervical osteomyelitis caused by Pseudomonas cepacia in an intravenous-drug abuser. J Clin Microbiol. 1985. 21:445–446.
Article7. Wertheim WA, Markovitz DM. Osteomyelitis and intervertebral discitis caused by Pseudomonas pickettii. J Clin Microbiol. 1992. 30:2506–2508.
Article8. Sudo H, Hisada Y, Ito M, Kotaki H, Minami A. Burkholderia pickettii spondylitis. Spinal Cord. 2005. 43:499–502.9. Alfonso Olmos M, Silva González A, Duart Clemente J, Villas Tomé C. Infected vertebroplasty due to uncommon bacteria solved surgically: a rare and threatening life complication of a common procedure: report of a case and a review of the literature. Spine (Phila Pa 1976). 2006. 31:E770–E773.10. Weinstein L, Knowlton CA, Smith MA. Cervical osteomyelitis caused by Burkholderia cepacia after rhinoplasty. J Infect Dev Ctries. 2008. 2:76–77.11. Huang CH, Jang TN, Liu CY, Fung CP, Yu KW, Wong WW. Characteristics of patients with Burkholderia cepacia bacteremia. J Microbiol Immunol Infect. 2001. 34:215–219.12. Sader HS, Jones RN. Antimicrobial susceptibility of uncommonly isolated non-enteric Gram-negative bacilli. Int J Antimicrob Agents. 2005. 25:95–109.
Article13. Lu DC, Chang SC, Chen YC, Luh KT, Hsieh WC. In vitro activities of antimicrobial agents, alone and in combinations, against Burkholderia cepacia isolated from blood. Diagn Microbiol Infect Dis. 1997. 28:187–191.
Article14. Bonacorsi S, Fitoussi F, Lhopital S, Bingen E. Comparative in vitro activities of meropenem, imipenem, temocillin, piperacillin, and ceftazidime in combination with tobramycin, rifampin, or ciprofloxacin against Burkholderia cepacia isolates from patients with cystic fibrosis. Antimicrob Agents Chemother. 1999. 43:213–217.
Article15. Zimmerli W. Clinical practice. Vertebral osteomyelitis. N Engl J Med. 2010. 362:1022–1029.16. MacGregor RR, Gibson GA, Bland JA. Imipenem pharmacokinetics and body fluid concentrations in patients receiving high-dose treatment for serious infections. Antimicrob Agents Chemother. 1986. 29:188–192.
Article17. Leigh DA, Griggs J, Tighe CM, Powell HD, Church JC, Wise K, Channon G, Curtis LB. Pharmacokinetic study of ceftazidime in bone and serum of patients undergoing hip and knee arthroplasty. J Antimicrob Chemother. 1985. 16:637–642.
Article18. Saux MC, Le Rebeller A, Leng B, Mintrosse J. Bone diffusion of trimethoprim and sulfamethoxazole high pressure liquid chromatography (HPLC). Pathol Biol (Paris). 1982. 30:385–388.19. Lewin C, Doherty C, Govan J. In vitro activities of meropenem, PD 127391, PD 131628, ceftazidime, chloramphenicol, cotrimoxazole, and ciprofloxacin against Pseudomonas cepacia. Antimicrob Agents Chemother. 1993. 37:123–125.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Burkholderia cepacia Pneumonia after Lung Transplantation in a Recipient without Cystic Fibrosis
- A case of lung abscess caused by Burkholderia cepacia in healthy child
- Two Case of Burkholderia cepacia Sepsis
- Burkholderia Cepacia Causing Nosocomial Urinary Tract Infection in Children
- Vertebral Osteomyelitis caused by Burkholderia cepacia in an Immunocompetent Elderly Patient After Acupuncture