Infect Chemother.
2010 Dec;42(6):407-410. 10.3947/ic.2010.42.6.407.
A Case Report on Successful Nonsurgical Treatment Using Antibiotics Alone in Aortic Stent Infection Diagnosed by Positron Emission Tomography
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University, College of Medicine, Seoul, Korea. heechoi@ewha.ac.kr
- 2Department of Radiology, Ewha Womans University, College of Medicine, Seoul, Korea.
- KMID: 2170321
- DOI: http://doi.org/10.3947/ic.2010.42.6.407
Abstract
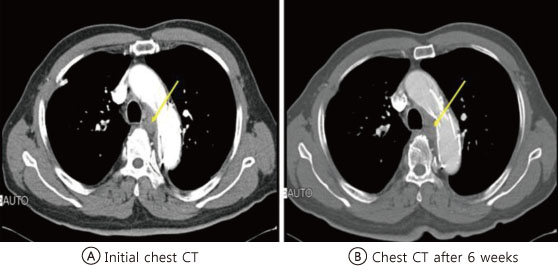
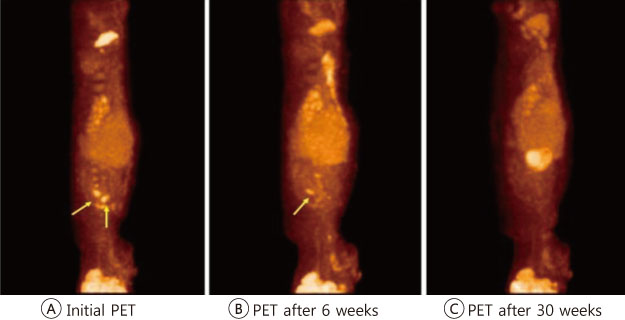
- Aortic stent infection is a rare problem, but severe sequelae such as stent occlusion, aortic necrosis and rupture, and life-threatening sepsis can occur. Surgical removal and antibiotic therapy has been the mainstay of treatment, but the management of stent infection still remains controversial as to the time of removal operation or the prognosis regarding the use of antibiotics alone as the treatment modality. Recently, we experienced a case of delayed aortic stent infection that was treated with antibiotics alone. A 68-year-old man presented with unexplained fever of several days' duration. The patient had a history of having had an aortic stent inserted 8 years ago due to traumatic aortic rupture. Blood culture was positive for Staphylococcus aureus and positron emission tomography revealed focal intense nodular uptake at medial and inferior aspect of the aortic arch. He was therefore diagnosed with aortic stent infection due to Staphylococcus aureus and was successfully treated with name of antibiotics alone without recourse to surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Myles O, Thomas WJ, Daniels JT, Aronson N. Infected endovascular stents managed with medical therapy alone. Catheter Cardiovasc Interv. 2000. 51:471–476.
Article2. Baddour LM, Bettmann MA, Bolger AF, Epstein AE, Ferrieri P, Gerber MA, Gewitz MH, Jacobs AK, Levison ME, Newburger JW, Pallasch TJ, Wilson WR, Baltimore RS, Falace DA, Shulman ST, Tani LY, Taubert KA. AHA. Nonvalvular cardiovascular device-related infections. Circulation. 2003. 108:2015–2031.
Article3. Dosluoglu HH, Curl GR, Doerr RJ, Painton F, Shenoy S. Stent-related iliac artery and iliac vein infections: two unreported presentations and review of the literature. J Endovasc Ther. 2001. 8:202–209.
Article4. Fukuchi K, Ishida Y, Higashi M, Tsunekawa T, Ogino H, Minatoya K, Kiso K, Naito H. Detection of aortic graft infection by fluorodeoxyglucose positron emission tomography: comparison with computed tomographic findings. J Vasc Surg. 2005. 42:919–925.
Article5. Therasse E, Soulez G, Cartier P, Passerini L, Roy P, Bruneau L, Gaboury L. Infection with fatal outcome after endovascular metallic stent placement. Radiology. 1994. 192:363–365.
Article6. Palmaz JC. Intravascular stents: tissue-stent interactions and design considerations. AJR Am J Roentgenol. 1993. 160:613–618.
Article7. Thibodeaux LC, James KV, Lohr JM, Welling RE, Roberts WH. Infection of endovascular stents in a swine model. Am J Surg. 1996. 172:151–154.
Article8. Naddour F, Yount RD Jr, Quintal RE. Successful conservative treatment of an infected central venous stent. Catheter Cardiovasc Interv. 2000. 51:196–198.
Article9. Hoffman M, Baruch R, Kaplan E, Mittelman M, Aviram G, Siegman-Igra Y. Coronary stent bacterial infection with multiple organ septic emboli. Eur J Intern Med. 2005. 16:123–125.
Article10. Kim DI, Lee BM, Lee JW, Cho KH, Jo YC, Shin JW, Lee MS. A case of probable endotipsitis after transjugular intrahepatic portasystemic shunt. Korean J Med. 2006. 70:232–236.11. Gonda E, Edmundson A, Mann T. Late coronary stent infection: a unique complication after drug-eluting stent implantation. J Invasive Cardiol. 2007. 19:E307–E308.12. Perera GB, Fujitani RM, Kubaska SM. Aortic graft infection: update on management and treatment options. Vasc Endovascular Surg. 2006. 40:1–10.
Article13. Zetrenne E, McIntosh BC, McRae MH, Gusberg R, Evans GR, Narayan D. Prosthetic vascular graft infection: a multi-center review of surgical management. Yale J Biol Med. 2007. 80:113–121.14. Chambers ST. Diagnosis and management of staphylococcal infections of vascular grafts and stents. Intern Med J. 2005. 35:Suppl 2. S72–S78.
Article15. Stádler P, Bìlohlávek O, Spacek M, Michálek P. Diagnosis of vascular prosthesis infection with FDG-PET/CT. J Vasc Surg. 2004. 40:1246–1247.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Graft Infection Using FDG PET-CT
- A Case of Stent Graft Infection Coupled With Aorto-Esophageal Fistula Following Thoracic Endovascular Aortic Repair in a Complex Patient
- Role of PET/CT in the Evaluation of Aortic Disease
- Oral cancer diagnosed using PET/CT: A case report
- A Case of an Infected Aneurysm in the Thoracic Aorta Mimicking Tuberculous Lymphadenopathy