Endocrinol Metab.
2011 Dec;26(4):340-344. 10.3803/EnM.2011.26.4.340.
Laparoscopically Resected Composite Pheochromocytoma-Ganglioneuroma
- Affiliations
-
- 1Department of Pathology, Gachon University Gil Hospital, Incheon, Korea. hicho@gilhospital.com
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Surgery, Gachon University Gil Hospital, Incheon, Korea.
- 4Division of Endocrinology and Metabolism, Department of Internal Medicine, Gachon University Gil Hospital, Incheon, Korea.
- KMID: 2169266
- DOI: http://doi.org/10.3803/EnM.2011.26.4.340
Abstract
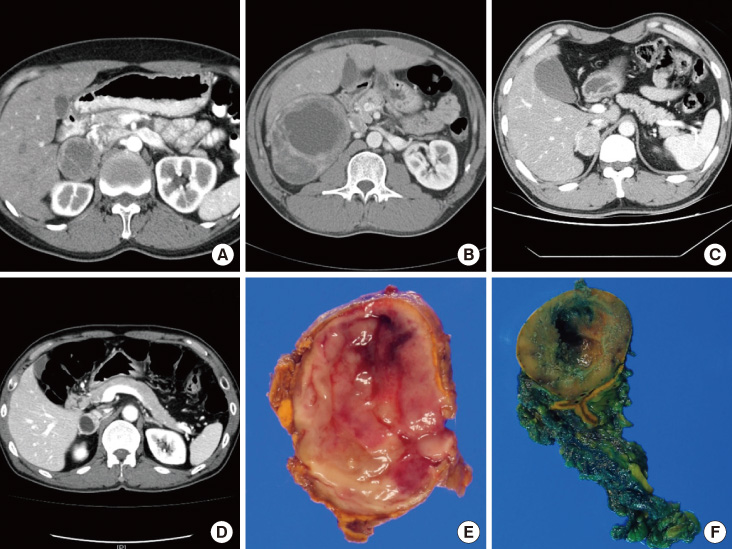
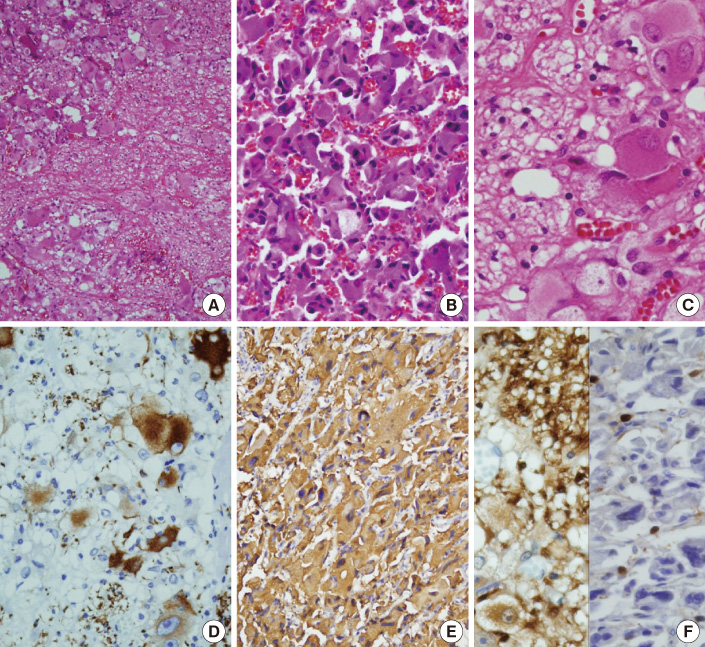
- Composite pheochromocytoma-ganglioneuroma is one of the mixed neuroendocrine-neural tumors composed of pheochromocytoma and other neural crest derivatives. To date, less than 50 cases of composite pheochromocytoma have been reported, and about 70% of the accompanying tumors were ganglioneuromas. Here, we describe six cases of composite pheochromocytoma-ganglioneuromas in five men and one woman, aged 33 to 64. The size of the tumors ranged from 3.0 to 11.0 cm, and four out of the six presented with intermittent onset of hypertension, palpitation, or dizziness. Microscopically, each tumor was composed of large pleomorphic shaped chromaffin cells arranged in the Zellballen patterns characteristic of pheochromocytoma, and they were mixed with clusters of mature ganglion cells and bundles of spindle-shaped Schwann cells characteristic of ganglioneuroma of variable proportions. All were successfully treated laparoscopically, and none were associated with multiple endocrine neoplasm syndrome or neurofibromatosis. Preoperative diagnosis of a composite pheochromocytoma-ganglioneuroma is impossible because of the low incidence rate, and the radiological findings and symptoms are similar to those of typical pheochromocytomas. Although the significance of microscopic detection of the nonpheochromocytoma component from pheochromocytoma has not yet been clarified, microscopic identification of the composite pheochromocytoma-ganglioneuroma is important because cumulative cases are used in an effort to predict the behavior of this composite tumor.
MeSH Terms
Figure
Reference
-
1. Menon S, Mahajan P, Desai SB. Composite adrenal medullary tumor: a rare cause of hypertension in a young male. Urol Ann. 2011. 3:36–38.2. Lau SK, Chu PG, Weiss LM. Mixed cortical adenoma and composite pheochromocytoma-ganglioneuroma: an unusual corticomedullary tumor of the adrenal gland. Ann Diagn Pathol. 2011. 15:185–189.3. George DJ, Watermeyer GA, Levin D, Epstein D, Ross IL, Scholz BU, Setshedi M, Locketz M, Dittrich C, Shaw J, Krige JE. Composite adrenal phaeochromocytoma-ganglioneuroma causing watery diarrhoea, hypokalaemia and achlorhydria syndrome. Eur J Gastroenterol Hepatol. 2010. 22:632–634.4. Gupta R, Sharma A, Arora R, Vijayaraghavan M. Composite phaeochromocytoma with malignant peripheral nerve sheath tumour and rhabdomyosarcomatous differentiation in a patient without von Recklinghausen disease. J Clin Pathol. 2009. 62:659–661.5. Choi EK, Kim WH, Park KY. A case of a composite adrenal medullary tumor of pheochromocytoma and ganglioneuroma masquerading as acute pancreatitis. Korean J Intern Med. 2006. 21:141–145.6. Ahn J, Lee SE, Chung YJ, Chi KC, Kim MK, Oh YS, Kim J. A case of papillary thyroid cancer and pheochromocytoma with ganglioneuroma. Korean J Med. 2009. 76:85–89.7. de Montpréville VT, Mussot S, Gharbi N, Dartevelle P, Dulmet E. Paraganglioma with ganglioneuromatous component located in the posterior mediastinum. Ann Diagn Pathol. 2005. 9:110–114.8. Khan AN, Solomon SS, Childress RD. Composite pheochromocytomaganglioneuroma: a rare experiment of nature. Endocr Pract. 2010. 16:291–299.9. Aiba M, Hirayama A, Ito Y, Fujimoto Y, Nakagami Y, Demura H, Shizume K. A compound adrenal medullary tumor (pheochromocytoma and ganglioneuroma) and a cortical adenoma in the ipsilateral adrenal gland. A case report with enzyme histochemical and immunohistochemical studies. Am J Surg Pathol. 1988. 12:559–566.10. Mahajan H, Lee D, Sharma R, Chin P, Watt WH, McBride G, Bilous M. Composite phaeochromocytoma-ganglioneuroma, an uncommon entity: report of two cases. Pathology. 2010. 42:295–298.11. Onozawa M, Fukuhara T, Minoguchi M, Takahata M, Yamamoto Y, Miyake T, Kanagawa K, Kanda M, Maekawa I. Hypokalemic rhabdomyolysis due to WDHA syndrome caused by VIP-producing composite pheochromocytoma: a case in neurofibromatosis type 1. Jpn J Clin Oncol. 2005. 35:559–563.12. Charfi S, Ayadi L, Ellouze S, Ghorbel R, Khabir A, Gouiaa N, Bahri I, Fakhfakh I, Makni S, Sellami-Boudawra T. Composite pheochromocytoma associated with multiple endocrine neoplasia type 2B. Ann Pathol. 2008. 28:225–228.13. Kragel PJ, Johnston CA. Pheochromocytoma-ganglioneuroma of the adrenal. Arch Pathol Lab Med. 1985. 109:470–472.14. Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR. The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev. 2004. 25:309–340.15. Lam KY, Lo CY. Composite pheochromocytoma-ganglioneuroma of the adrenal gland: an uncommon entity with distinctive clinicopathologic features. Endocr Pathol. 1999. 10:343–352.16. Lisewski D, Ryan S, Lim EM, Frost F, Nguyen H. Concomitant composite adrenal pheochromocytoma, multipte gastric stromal tumours and pseudohermaphrodism in a patient with von Recklinghausen's disease. Int Semin Surg Oncol. 2006. 3:11.17. Comstock JM, Willmore-Payne C, Holden JA, Coffin CM. Composite pheochromocytoma: a clinicopathologic and molecular comparison with ordinary pheochromocytoma and neuroblastoma. Am J Clin Pathol. 2009. 132:69–73.18. Kim HH, Kim GH, Sung GT. Laparoscopic adrenalectomy for pheochromocytoma: comparison with conventional open adrenalectomy. J Endourol. 2004. 18:251–255.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of a Composite Adrenal Medullary Tumor of Pheochromocytoma and Ganglioneuroma Masquerading as Acute Pancreatitis
- Composite Pheochromocytoma or Paraganglioma of Adrenal Gland: A Case Report with Immunohistochemical Studies and Electron Microscopic Examination
- A case of papillary thyroid cancer and pheochromocytoma with ganglioneuroma
- A Case of Ganglioneuroma Arising from the Retroperitoneal Sympathetic Chains
- A Case of Adrenal Ganglioneuroma