Allergy Asthma Respir Dis.
2015 May;3(3):228-231. 10.4168/aard.2015.3.3.228.
Eosinophilic gastroenteritis which leads to mal-absorption and anemia associated with food allergies
- Affiliations
-
- 1Department of Internal Medicine, Ajou University Hospital, Suwon, Korea. drsys93@naver.com
- 2Department of Allergy and Clinical Immunology, Ajou University Hospital, Suwon, Korea.
- KMID: 2168495
- DOI: http://doi.org/10.4168/aard.2015.3.3.228
Abstract
- Eosinophilic gastroenteritis (EG) is a rare disease characterized by massive eosinophilic infiltration of gastrointestinal tissue, peripheral eosinophilia, and nonspecific gastrointestinal symptoms. The mucosal type of EG commonly presented with malabsorption and anemia. However, the role of food allergy as a stimulus to EG has not yet been clearly defined. A 27-year-old man was referred to the Emergency Department with dyspepsia and leg swelling. The initial laboratory test should as follows: hemoglobin level, 6.4 g/dL; white blood cell count, 7,400/microL with 24.4% of eosinophil fraction; serum total protein, 3.9 g/dL; albumin level, 2.8 g/dL. Gastric endoscopy ruled out gastrointestinal bleeding showed multiple nodular raised lesions on the gastric antrum, which revealed increased eosinophilic infiltration (above 100/high power field). He had experienced nausea whenever eating beef, porks or fish. High serum specific IgE levels to offending foods (beef, 0.82 kU/L; pork, 0.83 kU/L; egg white, 0.40 kU/L; egg yolk, 0.54 kU/L; milk, 0.81 kU/L) were noted. He was instructed strictly to avoid food allergens with oral prednisolone therapy. Approximately 6 months after offending food restriction, the eosinophil count fell down to 400/microL, the hemoglobin level was returned to 11.5 g/dL and the serum albumin level was increased to 4.1 g/dL. We report a case of EG caused by multiple food allergy which leads to malabsorption and iron-deficiency anemia.
MeSH Terms
-
Adult
Allergens
Anemia*
Anemia, Iron-Deficiency
Dyspepsia
Eating
Egg White
Egg Yolk
Emergency Service, Hospital
Endoscopy
Eosinophilia
Eosinophils*
Food Hypersensitivity*
Gastroenteritis*
Hemorrhage
Humans
Immunoglobulin E
Leg
Leukocyte Count
Malabsorption Syndromes
Milk
Nausea
Prednisolone
Pyloric Antrum
Rare Diseases
Serum Albumin
Allergens
Immunoglobulin E
Prednisolone
Serum Albumin
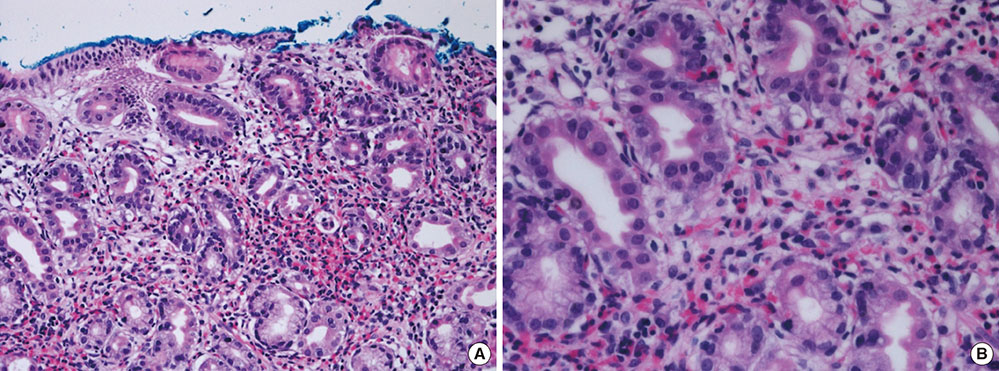
Figure
Reference
-
1. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004; 113:11–28.
Article2. Min KU, Metcalf DD. Eosinophilic gastroenteritis. Immunol Allergy Clin North Am. 1991; 11:799–813.3. Kagalwalla AF, Sentongo TA, Ritz S, Hess T, Nelson SP, Emerick KM, et al. Effect of six-food elimination diet on clinical and histologic outcomes in eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2006; 4:1097–1102.
Article4. Gonsalves N, Yang GY, Doerfler B, Ritz S, Ditto AM, Hirano I. Elimination diet effectively treats eosinophilic esophagitis in adults; food reintroduction identifies causative factors. Gastroenterology. 2012; 142:1451–1459.e1.
Article5. Yamada Y, Kato M, Isoda Y, Nishi A, Jinbo Y, Hayashi Y. Eosinophilic gastroenteritis treated with a multiple-food elimination diet. Allergol Int. 2014; 63:Suppl 1. 53–56.
Article6. Rodriguez Jimenez B, Dominguez Ortega J, Gonzalez Garcia JM, Kindelan Recarte C. Eosinophilic gastroenteritis due to allergy to cow's milk. J Investig Allergol Clin Immunol. 2011; 21:150–152.7. Suzuki S, Homma T, Kurokawa M, Matsukura S, Adachi M, Wakabayashi K, et al. Eosinophilic gastroenteritis due to cow's milk allergy presenting with acute pancreatitis. Int Arch Allergy Immunol. 2012; 158:Suppl 1. 75–82.
Article8. Park HS, Kim HS, Jang HJ. Eosinophilic gastroenteritis associated with food allergy and bronchial asthma. J Korean Med Sci. 1995; 10:216–219.
Article9. Kim NI, Jo YJ, Song MH, Kim SH, Kim TH, Park YS, et al. Clinical features of eosinophilic gastroenteritis. Korean J Gastroenterol. 2004; 44:217–223.10. Kaijser R. Allergic diseases of the gut from the point of view of the surgeon. Arch Klin Chir. 1937; 188:36–64.11. Jeon EJ, Lee KM, Jung DY, Kim TH, Ji JS, Kim HK, et al. Clinical characteristics of 17 cases of eosinophilic gastroenteritis. Korean J Gastroenterol. 2010; 55:361–367.
Article12. Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970; 49:299–319.
Article13. Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. 1990; 31:54–58.
Article14. Katz AJ, Twarog FJ, Zeiger RS, Falchuk ZM. Milk-sensitive and eosinophilic gastroenteropathy: similar clinical features with contrasting mechanisms and clinical course. J Allergy Clin Immunol. 1984; 74:72–78.
Article15. Chruszcz M, Mikolajczak K, Mank N, Majorek KA, Porebski PJ, Minor W. Serum albumins-unusual allergens. Biochim Biophys Acta. 2013; 1830:5375–5381.
Article16. Orhan F, Sekerel BE. Beef allergy: a review of 12 cases. Allergy. 2003; 58:127–131.
Article17. Commins SP, Satinover SM, Hosen J, Mozena J, Borish L, Lewis BD, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009; 123:426–433.18. Kim JH, An S, Kim JE, Choi GS, Ye YM, Park HS. Beef-induced anaphylaxis confirmed by the basophil activation test. Allergy Asthma Immunol Res. 2010; 2:206–208.
Article