Ann Surg Treat Res.
2015 Oct;89(4):183-189. 10.4174/astr.2015.89.4.183.
Influence of old age on the postoperative outcomes of obstructive colorectal cancer surgery after the insertion of a stent
- Affiliations
-
- 1Department of Surgery, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. shinycloud@dsmc.or.kr
- KMID: 2166887
- DOI: http://doi.org/10.4174/astr.2015.89.4.183
Abstract
- PURPOSE
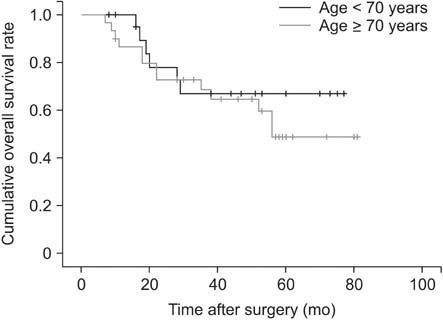
In some patients more than 70 years of age with obstructive colorectal cancer, their concerns about the postoperative complications lead them to refuse surgery after the insertion of a stent. This study aimed to compare the postoperative outcomes between obstructive colorectal cancer patients aged less than 70 years and those aged 70 years and more who underwent surgery after the insertion of a colonoscopic stent.
METHODS
Patients with obstructive colorectal cancer who underwent surgery after the insertion of a colonoscopic stent between March 2004 and March 2014 were reviewed retrospectively by using medical records. The patients were divided into two groups: 22 patients were aged less than 70 years (group A) and 30 patients were aged more than 70 years (group B).
RESULTS
Although no significant difference in comorbidity was noted between the two groups, the American Society of Anesthesiologists (ASA) score was higher in group B. There was no significant difference in cancer location, stage, or the time from the insertion of the stent to operation. The perioperative results including operation time, blood loss, and length of stay were not significantly different between the groups. The postoperative complications were also not significantly different.
CONCLUSION
The surgical outcomes of elderly patients were similar to those of younger patients, despite higher ASA scores. These results indicate that surgery can be performed safely in elderly patients with obstructive colorectal cancer after the insertion of a stent.
Keyword
MeSH Terms
Figure
Reference
-
1. Rutten HJ, den Dulk M, Lemmens VE, van de Velde CJ, Marijnen CA. Controversies of total mesorectal excision for rectal cancer in elderly patients. Lancet Oncol. 2008; 9:494–501.2. Shin A, Kim KZ, Jung KW, Park S, Won YJ, Kim J, et al. Increasing trend of colorectal cancer incidence in Korea, 1999-2009. Cancer Res Treat. 2012; 44:219–226.3. Tan CJ, Dasari BV, Gardiner K. Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg. 2012; 99:469–476.4. Bonin EA, Baron TH. Update on the indications and use of colonic stents. Curr Gastroenterol Rep. 2010; 12:374–382.5. Dulucq JL, Wintringer P, Beyssac R, Barberis C, Talbi P, Mahajna A. One-stage laparoscopic colorectal resection after placement of self-expanding metallic stents for colorectal obstruction: a prospective study. Dig Dis Sci. 2006; 51:2365–2371.6. Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2012; 26:110–119.7. Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg. 2005; 140:278–283.8. Evers BM, Townsend CM Jr, Thompson JC. Organ physiology of aging. Surg Clin North Am. 1994; 74:23–39.9. Polanczyk CA, Marcantonio E, Goldman L, Rohde LE, Orav J, Mangione CM, et al. Impact of age on perioperative complications and length of stay in patients undergoing noncardiac surgery. Ann Intern Med. 2001; 134:637–643.10. Eguchi T, Takahashi Y, Ikarashi M, Kasahara M, Fujii M. Is extended lymph node dissection necessary for gastric cancer in elderly patients? Eur J Surg. 2000; 166:949–953.11. Hayashi T, Yoshikawa T, Aoyama T, Ogata T, Cho H, Tsuburaya A. Severity of complications after gastrectomy in elderly patients with gastric cancer. World J Surg. 2012; 36:2139–2145.12. Maehara Y, Oshiro T, Oiwa H, Oda S, Baba H, Akazawa K, et al. Gastric carcinoma in patients over 70 years of age. Br J Surg. 1995; 82:102–105.13. Diamantini G, Rossi P, Caciolo F, Levi Sandri GB, Procacciante F. Colorectal surgery for cancer in very elderly patient. Int J Colorectal Dis. 2015; 30:1131–1132.14. Kockerling F, Rose J, Schneider C, Scheidbach H, Scheuerlein H, Reymond MA, et al. Laparoscopic Colorectal Surgery Study Group (LCSSG). Laparoscopic colorectal anastomosis: risk of postoperative leakage. Results of a multicenter study. Surg Endosc. 1999; 13:639–644.15. Ceulemans R, Al-Ahdab N, Leroy J, Garcia A, Dutson E, Rubino F, et al. Safe laparoscopic surgery in the elderly. Am J Surg. 2004; 187:323–327.16. Kronberg U, Kiran RP, Soliman MS, Hammel JP, Galway U, Coffey JC, et al. A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg. 2011; 253:78–81.17. Chapuis PH, Bokey L, Keshava A, Rickard MJ, Stewart P, Young CJ, et al. Risk factors for prolonged ileus after resection of colorectal cancer: an observational study of 2400 consecutive patients. Ann Surg. 2013; 257:909–915.18. Vallribera Valls F, Landi F, Espin Basany E, Sanchez Garcia JL, Jimenez Gomez LM, Marti Gallostra M, et al. Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: morbidity and mortality outcomes in 545 patients. Surg Endosc. 2014; 28:3373–3378.19. Hinoi T, Kawaguchi Y, Hattori M, Okajima M, Ohdan H, Yamamoto S, et al. Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol. 2015; 22:2040–2050.20. Jimenez-Perez J, Casellas J, Garcia-Cano J, Vandervoort J, Garcia-Escribano OR, Barcenilla J, et al. Colonic stenting as a bridge to surgery in malignant large-bowel obstruction: a report from two large multinational registries. Am J Gastroenterol. 2011; 106:2174–2180.21. Abdussamet Bozkurt M, Gonenc M, Kapan S, Kocatass A, Temizgonul B, Alis H. Colonic stent as bridge to surgery in patients with obstructive left-sided colon cancer. JSLS. 2014; Oct-Dec. 18:pii: e2014.00161.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Resection after Stenting in Obstructive Colorectal Cancers
- Is stent insertion for obstructing colon cancer a good prognostic factor in long-term oncologic outcomes in symptomatic obstructive colon cancer?
- Short-term Oncologic Outcome of Curative Resection for Obstructive Colorectal Cancer Followed by Stent Insertion: Comparative Study with Non-abstructive Colorectal Cancer
- Laparoscopic Colorectal Resection after Endoscopic Stent Insertion in Cases of Malignant Colorectal Obstruction: the Experience of a Single Center
- Short-Term Outcome of Curative One-Stage Laparoscopic Resection for Obstructive Left-Sided Colon Cancers Followed by Stent Insertion: Comparative Study with Non-Obstructive Left-Sided Colon Cancers