Ann Rehabil Med.
2015 Jun;39(3):409-415. 10.5535/arm.2015.39.3.409.
Analysis of Vertical Ground Reaction Force Variables Using Foot Scans in Hemiplegic Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. lime980@naver.com
- 2Department of Physical Medicine and Rehabilitation, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2165644
- DOI: http://doi.org/10.5535/arm.2015.39.3.409
Abstract
OBJECTIVE
To analyze the differences in the vertical ground reaction force (GRF) variables of hemiplegic patients compared with a control group, and between the affected and unaffected limbs of hemiplegic patients using foot scans.
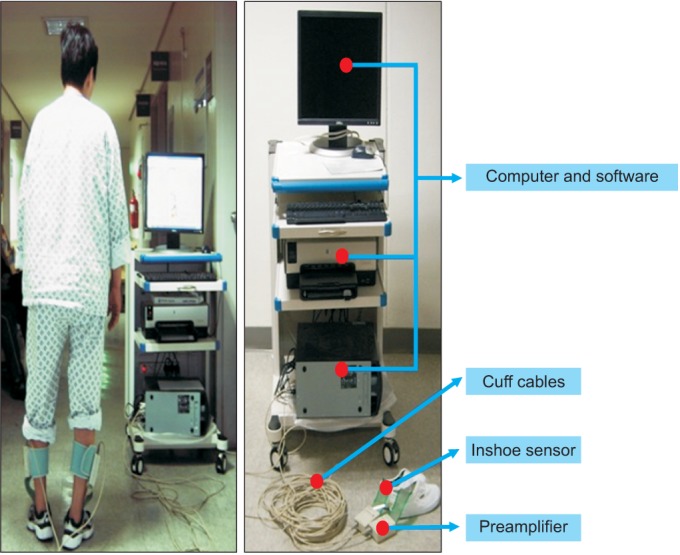
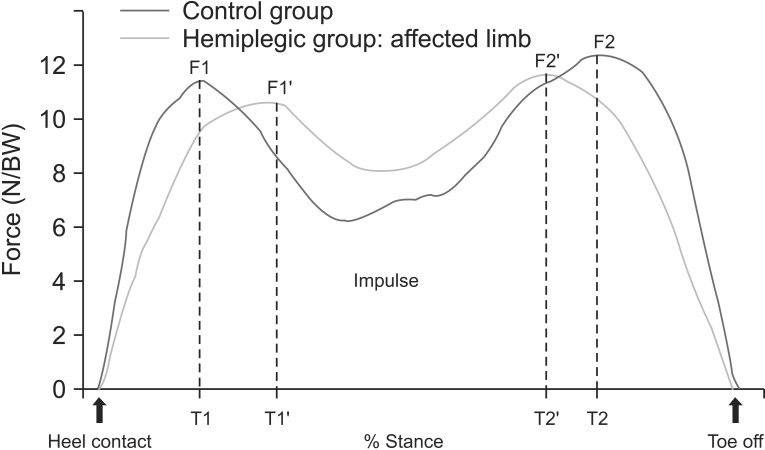
METHODS
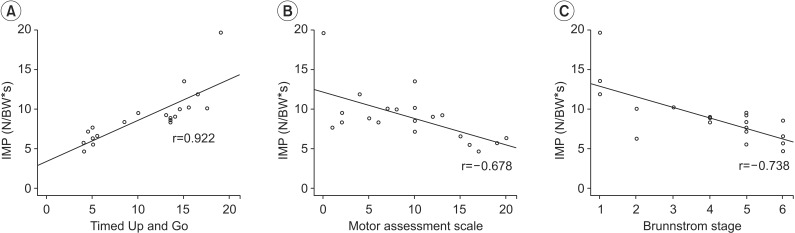
Patients (n=20) with hemiplegia and healthy volunteers (n=20) underwent vertical force analysis. We measured the following: the first and second peak forces (F1, F2) and the percent stances at which they occurred (T1, T2); the vertical force impulse (VFI) and stance times. The GRF results were compared between the hemiplegic patients and control individuals, and between the affected and unaffected limbs of hemiplegic patients. Additionally, we analyzed the impulse of the unaffected limb according to the motor assessment scale (MAS), Brunnstrom stage, and a Timed Up and Go Test.
RESULTS
The F1s and F2s of the affected and unaffected limbs were significantly less than those of the normal control individuals (p<0.05). The T1s of both the affected and unaffected limbs of the patients were greater than control individuals, whilst the T2s were lower (p<0.05). Greater impulses and stance times were recorded on both sides of the patients than in the limbs of the control individuals (p<0.05). The MAS, Brunnstrom stage and Timed Up and Go Test results were significantly correlated with the VFI of the unaffected limbs (p<0.05).
CONCLUSION
The high impulse values of the unaffected limb were associated with complications during gait rehabilitation. Therefore, these results suggest that unaffected limbs should also be taken into consideration in these patients.
Keyword
Figure
Cited by 1 articles
-
Comment on “Effect of Extracorporeal Shockwave Therapy Versus Intra-articular Injections of Hyaluronic Acid for the Treatment of Knee Osteoarthritis”
Valter Santilli, Federica Alviti, Marco Paoloni, Massimiliano Mangone, Andrea Bernetti
Ann Rehabil Med. 2018;42(2):372-373. doi: 10.5535/arm.2018.42.2.372.
Reference
-
1. Friedman PJ. Gait recovery after hemiplegic stroke. Int Disabil Stud. 1990; 12:119–122. PMID: 2096120.
Article2. Park JW, Park SH, Ko MH. Change of plantar fascia thickness in hemiplegic patients. J Korean Soc Phys Ther. 2009; 21:41–46.3. Zadpoor AA, Nikooyan AA. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clin Biomech (Bristol, Avon). 2011; 26:23–28.
Article4. Higashi T, Funase K, Kusano K, Tabira T, Harada N, Sakakibara A, et al. Motoneuron pool excitability of hemiplegic patients: assessing recovery stages by using H-reflex and M response. Arch Phys Med Rehabil. 2001; 82:1604–1610. PMID: 11689982.
Article5. Tucak C, Scott J, Kirkman A, Singer B. Relationships between initial Motor Assessment Scale scores and length of stay, mobility at discharge and discharge destination after stroke. NZ J Physiother. 2010; 38:7–13.6. Ng SS, Hui-Chan CW. The timed up & go test: its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch Phys Med Rehabil. 2005; 86:1641–1647. PMID: 16084820.7. Mulroy S, Gronley J, Weiss W, Newsam C, Perry J. Use of cluster analysis for gait pattern classification of patients in the early and late recovery phases following stroke. Gait Posture. 2003; 18:114–125. PMID: 12855307.
Article8. Bella GP, Rodrigues NB, Valenciano PJ, Silva LM, Souza RC. Correlation among the Visual Gait Assessment Scale, Edinburgh Visual Gait Scale and Observational Gait Scale in children with spastic diplegic cerebral palsy. Rev Bras Fisioter. 2012; 16:134–140. PMID: 22584771.9. Brown CR, Hillman SJ, Richardson AM, Herman JL, Robb JE. Reliability and validity of the Visual Gait Assessment Scale for children with hemiplegic cerebral palsy when used by experienced and inexperienced observers. Gait Posture. 2008; 27:648–652. PMID: 17913500.
Article10. Jonsdottir J, Cattaneo D. Reliability and validity of the dynamic gait index in persons with chronic stroke. Arch Phys Med Rehabil. 2007; 88:1410–1415. PMID: 17964880.
Article11. Sutherland DH. The evolution of clinical gait analysis part l: kinesiological EMG. Gait Posture. 2001; 14:61–70. PMID: 11378426.
Article12. Takebe K, Basmajian JV. Gait analysis in stroke patients to assess treatments of foot-drop. Arch Phys Med Rehabil. 1976; 57:305–310. PMID: 1084734.13. Tenore N, Fortugno F, Viola F, Galli M, Giaquinto S. Gait analysis as a reliable tool for rehabilitation of chronic hemiplegic patients. Clin Exp Hypertens. 2006; 28:349–355. PMID: 16833045.
Article14. Turani N, Kemiksizoglu A, Karatas M, Ozker R. Assessment of hemiplegic gait using the Wisconsin Gait Scale. Scand J Caring Sci. 2004; 18:103–108. PMID: 15005669.
Article15. Bertani A, Cappello A, Benedetti MG, Simoncini L, Catani F. Flat foot functional evaluation using pattern recognition of ground reaction data. Clin Biomech (Bristol, Avon). 1999; 14:484–493.
Article16. Chen G, Patten C, Kothari DH, Zajac FE. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture. 2005; 22:51–56. PMID: 15996592.
Article17. Morita S, Yamamoto H, Furuya K. Gait analysis of hemiplegic patients by measurement of ground reaction force. Scand J Rehabil Med. 1995; 27:37–42. PMID: 7792548.18. Orlin MN, McPoil TG. Plantar pressure assessment. Phys Ther. 2000; 80:399–409. PMID: 10758524.
Article19. Mizrahi J, Susak Z, Heller L, Najenson T. Objective expression of gait improvement of hemiplegics during rehabilitation by time-distance parameters of the stride. Med Biol Eng Comput. 1982; 20:628–634. PMID: 7176722.
Article20. Mizrahi J, Susak Z, Heller L, Najenson T. Variation of time-distance parameters of the stride as related to clinical gait improvement in hemiplegics. Scand J Rehabil Med. 1982; 14:133–140. PMID: 7134913.21. Wall JC, Ashburn A. Assessment of gait disability in hemiplegics. Hemiplegic gait. Scand J Rehabil Med. 1979; 11:95–103. PMID: 493898.22. Chen CY, Hong PW, Chen CL, Chou SW, Wu CY, Cheng PT, et al. Ground reaction force patterns in stroke patients with various degrees of motor recovery determined by plantar dynamic analysis. Chang Gung Med J. 2007; 30:62–72. PMID: 17477031.23. Kerrigan DC, Karvosky ME, Riley PO. Spastic paretic stiff-legged gait: joint kinetics. Am J Phys Med Rehabil. 2001; 80:244–249. PMID: 11277129.24. Horvath M, Tihanyi T, Tihanyi J. Kinematic and kinetic analyses of gait patterns in hemiplegic patients. Facta Univ Ser Physic Educ Sport. 2001; 1:25–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lower Extremity Biomechanical Comparison Analysis of Single Leg Drop Landing among Normal Foot and Flat Foot
- The Shoes Designed to Inhibit Excessive External Rotation of Hemiplegic Foot with Plastic Ankle Foot Orthosis: A case report
- The Effects of Foot Position on Dynamic Stability during Squat in Female with Genu Varum
- Correlation among Functional Leg Length Discrepancy, Muscle Activity, Muscle Contraction Onset Time and Vertical Ground Reaction Force during Simple Lifting Task
- Effect of Torque Heel on Excessive External Rotation of Hemiplegic Foot: Three Dimensional Gait Analysis