Brain Tumor Res Treat.
2013 Apr;1(1):50-53. 10.14791/btrt.2013.1.1.50.
A Suprasellar Cystic Germ Cell Tumor Initially Diagnosed as an Arachnoid Cyst
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. choihs1786@snubh.org
- 2Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 3Department of Radiation Oncology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- KMID: 2165224
- DOI: http://doi.org/10.14791/btrt.2013.1.1.50
Abstract
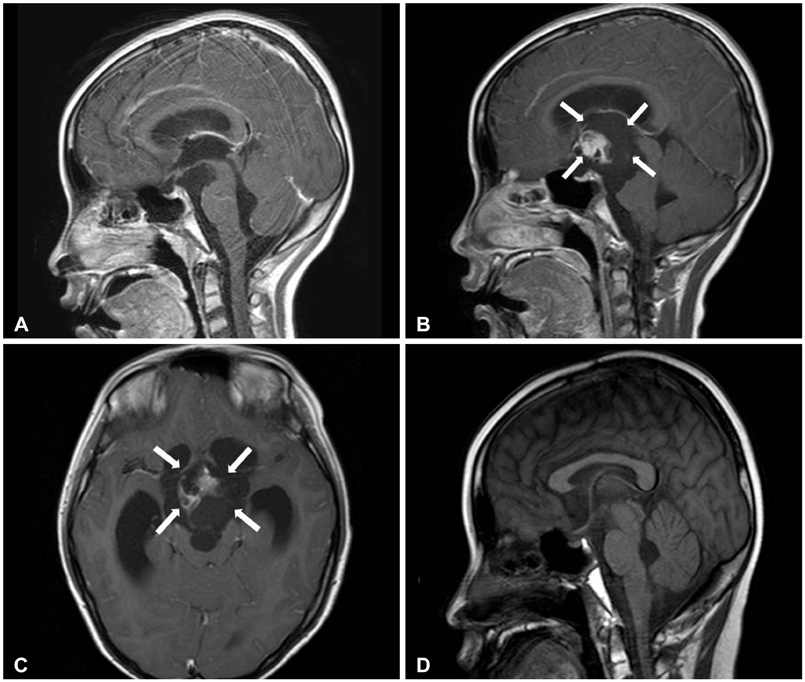
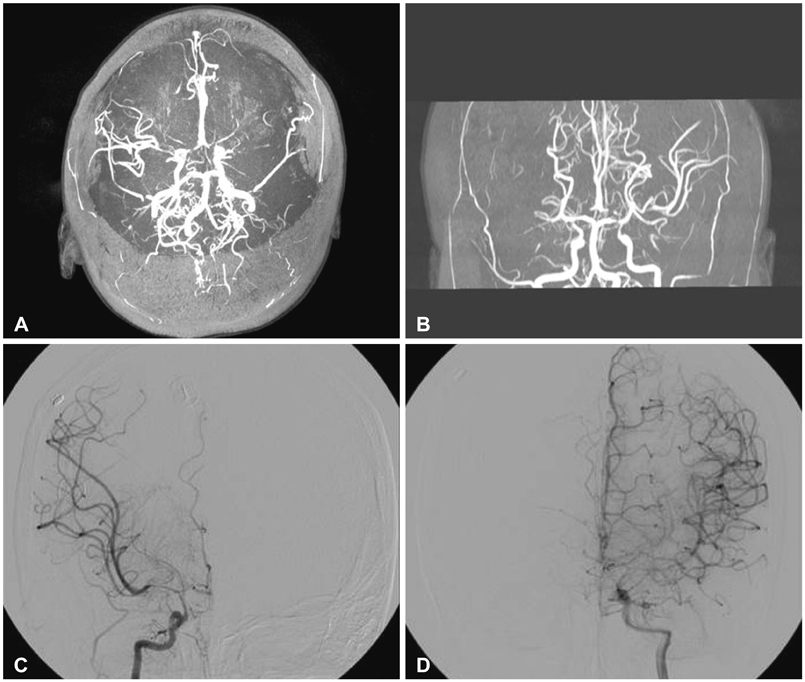
- We report here the case of a suprasellar cystic germ cell tumor (GCT) initially diagnosed as an arachnoid cyst. A 10-year-old boy experienced headache, dizziness, and diplopia, and was shown to have an approximately 2 cm suprasellar cyst. Two months after endoscopic third ventriculostomy was performed, a 5-6 cm cystic mass with an internal enhancing component was observed in the suprasellar cistern. Serum human chorionic gonadotropin levels were slightly increased in the serum and cerebrospinal fluid (55 and 162 IU/L, respectively) but were strikingly elevated in the cystic fluid (14,040 IU/L). The patient showed complete remission, with only a very small cystic lesion remaining after surgery, chemotherapy, and radiation treatment for a suprasellar mixed GCT. However, follow-up after treatment was complicated by moyamoya syndrome and cerebral infarction. GCT can be considered as a rare differential diagnosis in the case of a suprasellar cystic mass. Evaluation of tumor markers and close follow-up will be necessary.
MeSH Terms
-
Arachnoid*
Central Nervous System Cysts*
Cerebral Infarction
Cerebrospinal Fluid
Child
Chorionic Gonadotropin
Diagnosis, Differential
Diplopia
Dizziness
Drug Therapy
Follow-Up Studies
Germ Cells*
Headache
Humans
Male
Moyamoya Disease
Neoplasms, Germ Cell and Embryonal*
Biomarkers, Tumor
Ventriculostomy
Chorionic Gonadotropin
Tumor Markers, Biological
Figure
Reference
-
1. Echevarría ME, Fangusaro J, Goldman S. Pediatric central nervous system germ cell tumors: a review. Oncologist. 2008; 13:690–699.
Article2. Atlas M. Central nervous system malignancies. In : Lanzkowsky P, editor. Manual of Pediatric Hematology and Oncology. 5th ed. London: Academic Press;2011. p. 647–670.3. Fujimaki T. Central nervous system germ cell tumors: classification, clinical features, and treatment with a historical overview. J Child Neurol. 2009; 24:1439–1445.
Article4. Tihan T. Germ cell tumors. In : Adesina AM, Tihan T, Fuller CE, Poussaint TY, editors. Atlas of Pediatric Brain Tumors. New York: Springer;2010. p. 291–292.5. Liang L, Korogi Y, Sugahara T, et al. MRI of intracranial germ-cell tumours. Neuroradiology. 2002; 44:382–388.
Article6. Derman A, Shields M, Davis A, Knopp E, Fatterpekar GM. Diseases of the sella and parasellar region: an overview. Semin Roentgenol. 2013; 48:35–51.
Article7. Cincu R, Agrawal A, Eiras J. Intracranial arachnoid cysts: current concepts and treatment alternatives. Clin Neurol Neurosurg. 2007; 109:837–843.
Article8. Schroeder JW, Vezina LG. Pediatric sellar and suprasellar lesions. Pediatr Radiol. 2011; 41:287–298. quiz 404-5.
Article9. Ullrich NJ, Robertson R, Kinnamon DD, et al. Moyamoya following cranial irradiation for primary brain tumors in children. Neurology. 2007; 68:932–938.
Article10. Desai SS, Paulino AC, Mai WY, Teh BS. Radiation-induced moyamoya syndrome. Int J Radiat Oncol Biol Phys. 2006; 65:1222–1227.
Article