Clin Endosc.
2016 May;49(3):273-281. 10.5946/ce.2015.086.
Usefulness of the Forrest Classification to Predict Artificial Ulcer Rebleeding during Second-Look Endoscopy after Endoscopic Submucosal Dissection
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Soonchunhyang University College of Medicine, Cheonan, Korea. euschung@schmc.ac.kr
- KMID: 2165022
- DOI: http://doi.org/10.5946/ce.2015.086
Abstract
- BACKGROUND/AIMS
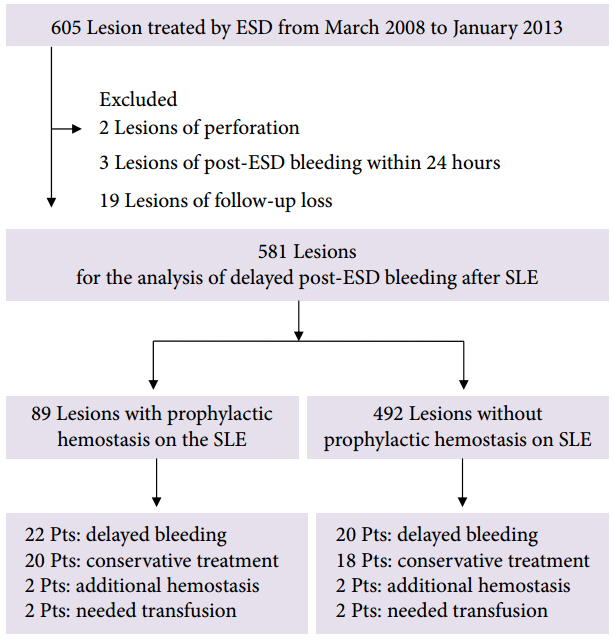
Delayed post-endoscopic submucosal dissection (ESD) bleeding (DPEB) is difficult to predict and there is controversy regarding the usefulness of prophylactic hemostasis during second-look endoscopy. This study evaluated the risk factors related to DPEB, the relationship between clinical outcomes and the Forrest classification, and the results of prophylactic hemostasis during second-look endoscopy.
METHODS
Second-look endoscopy was performed on the day after ESD to check for recent hemorrhage or potential bleeding and the presence of artificial ulcers in all patients.
RESULTS
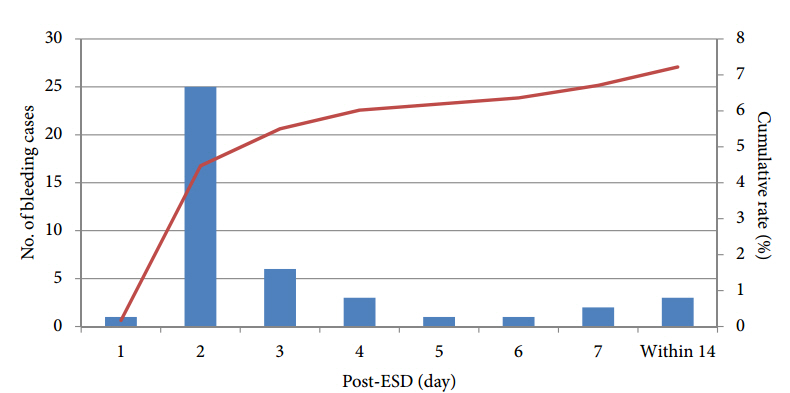
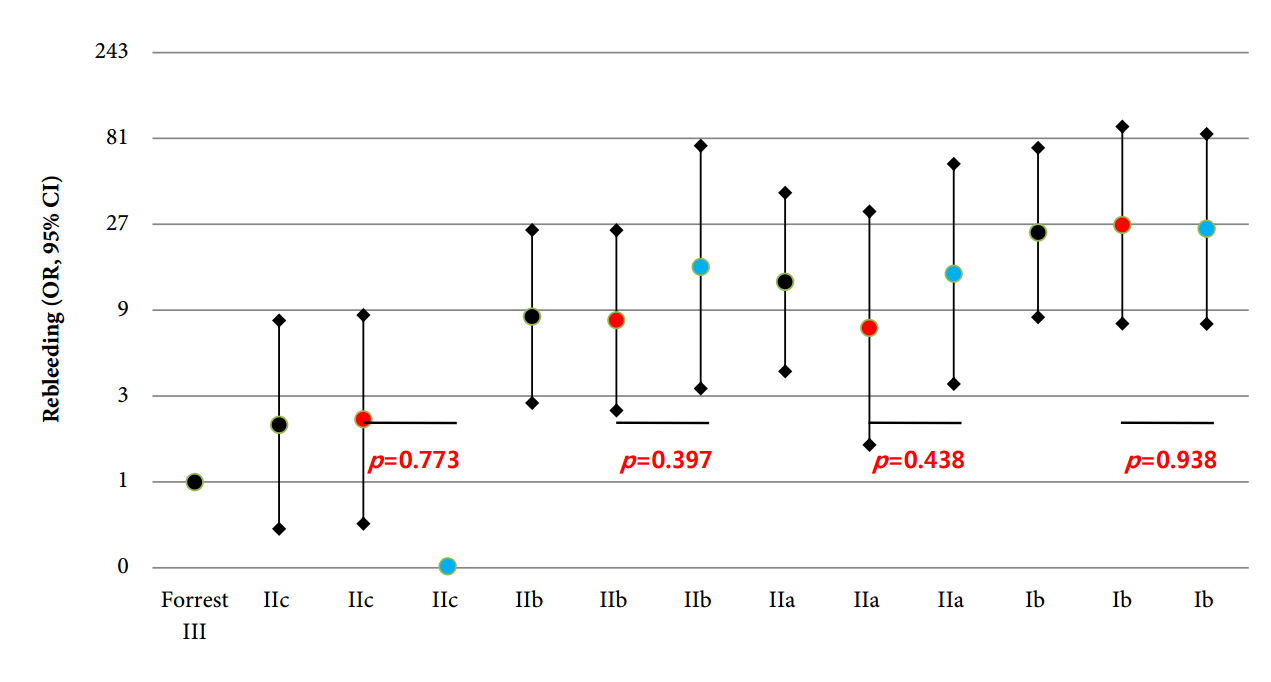
DPEB occurred in 42 of 581 patients (7.2%). Multivariate analysis determined that a specimen size ≥40 mm (odds ratio [OR], 3.03; p=0.003), and a high-risk Forrest classification (Forrest Ib+IIa+IIb; OR, 6.88; p<0.001) were risk factors for DPEB. DPEB was significantly more likely in patients classified with Forrest Ib (OR, 24.35; p<0.001), IIa (OR, 12.91; p<0.001), or IIb (OR, 8.31; p<0.001) ulcers compared with Forrest III ulcers. There was no statistically significant difference between the prophylactic hemostasis and non-hemostasis groups (Forrest Ib, p=0.938; IIa, p=0.438; IIb, p=0.397; IIc, p=0.773) during second-look endoscopy.
CONCLUSIONS
The Forrest classification of artificial gastric ulcers during second-look endoscopy seems to be a useful tool for predicting delayed bleeding. However, routine prophylactic hemostasis during second-look endoscopy seemed to not be useful for preventing DPEB.
MeSH Terms
Figure
Cited by 2 articles
-
Effectiveness of Autologous Platelet-Rich Plasma for the Healing of Ulcers after Endoscopic Submucosal Dissection
Eunju Jeong, In kyung Yoo, Ozlem Ozer Cakir, Hee Kyung Kim, Won Hee Kim, Sung Pyo Hong, Joo Young Cho
Clin Endosc. 2019;52(5):472-478. doi: 10.5946/ce.2018.152.Second-Look Endoscopy after Endoscopic Submucosal Dissection: Can We Obtain Valuable Information?
Hye Kyung Jeon, Gwang Ha Kim
Clin Endosc. 2016;49(3):212-213. doi: 10.5946/ce.2016.062.
Reference
-
1. Min YW, Min BH, Lee JH, Kim JJ. Endoscopic treatment for early gastric cancer. World J Gastroenterol. 2014; 20:4566–4573.
Article2. Gotoda T. Endoscopic resection of early gastric cancer. Gastric Cancer. 2007; 10:1–11.
Article3. Chung IK, Lee JH, Lee SH, et al. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009; 69:1228–1235.
Article4. Goto O, Fujishiro M, Kodashima S, et al. A second-look endoscopy after endoscopic submucosal dissection for gastric epithelial neoplasm may be unnecessary: a retrospective analysis of postendoscopic submucosal dissection bleeding. Gastrointest Endosc. 2010; 71:241–248.
Article5. Kim HH, Park SJ, Park MI, Moon W. Clinical impact of second-look endoscopy after endoscopic submucosal dissection of gastric neoplasms. Gut Liver. 2012; 6:316–320.
Article6. Ryu HY, Kim JW, Kim HS, et al. Second-look endoscopy is not associated with better clinical outcomes after gastric endoscopic submucosal dissection: a prospective, randomized, clinical trial analyzed on an as-treated basis. Gastrointest Endosc. 2013; 78:285–294.
Article7. Choi CW, Kim HW, Kang DH, et al. Clinical outcomes of second-look endoscopy after gastric endoscopic submucosal dissection: predictive factors with high risks of bleeding. Surg Endosc. 2014; 28:2213–2220.
Article8. Kim ER, Kim JH, Kang KJ, et al. Is a second-look endoscopy necessary after endoscopic submucosal dissection for gastric neoplasm? Gut Liver. 2015; 9:52–58.
Article9. Takizawa K, Oda I, Gotoda T, et al. Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection: an analysis of risk factors. Endoscopy. 2008; 40:179–183.10. Uedo N, Takeuchi Y, Yamada T, et al. Effect of a proton pump inhibitor or an H2-receptor antagonist on prevention of bleeding from ulcer after endoscopic submucosal dissection of early gastric cancer: a prospective randomized controlled trial. Am J Gastroenterol. 2007; 102:1610–1616.
Article11. Lee SH, Lee CK, Chung IK, et al. Optimal duration of proton pump inhibitor in the treatment of endoscopic submucosal dissection-induced ulcers: a retrospective analysis and prospective validation study. Dig Dis Sci. 2012; 57:429–434.
Article12. Goto O, Fujishiro M, Kodashima S, et al. Short-term healing process of artificial ulcers after gastric endoscopic submucosal dissection. Gut Liver. 2011; 5:293–297.
Article13. Muraki Y, Enomoto S, Iguchi M, Fujishiro M, Yahagi N, Ichinose M. Management of bleeding and artificial gastric ulcers associated with endoscopic submucosal dissection. World J Gastrointest Endosc. 2012; 4:1–8.
Article14. Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet. 1974; 2:394–397.
Article15. Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996; 38:316–321.
Article16. de Groot NL, van Oijen MG, Kessels K, et al. Reassessment of the predictive value of the Forrest classification for peptic ulcer rebleeding and mortality: can classification be simplified? Endoscopy. 2014; 46:46–52.
Article17. Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006; 41:929–942.
Article18. Mannen K, Tsunada S, Hara M, et al. Risk factors for complications of endoscopic submucosal dissection in gastric tumors: analysis of 478 lesions. J Gastroenterol. 2010; 45:30–36.
Article19. Okada K, Yamamoto Y, Kasuga A, et al. Risk factors for delayed bleeding after endoscopic submucosal dissection for gastric neoplasm. Surg Endosc. 2011; 25:98–107.
Article20. Villanueva C, Balanzó J, Torras X, Soriano G, Sáinz S, Vilardell F. Value of second-look endoscopy after injection therapy for bleeding peptic ulcer: a prospective and randomized trial. Gastrointest Endosc. 1994; 40:34–39.
Article21. Saeed ZA, Cole RA, Ramirez FC, Schneider FE, Hepps KS, Graham DY. Endoscopic retreatment after successful initial hemostasis prevents ulcer rebleeding: a prospective randomized trial. Endoscopy. 1996; 28:288–294.
Article22. Chiu PW, Lam CY, Lee SW, et al. Effect of scheduled second therapeutic endoscopy on peptic ulcer rebleeding: a prospective randomised trial. Gut. 2003; 52:1403–1407.
Article23. El Ouali S, Barkun AN, Wyse J, et al. Is routine second-look endoscopy effective after endoscopic hemostasis in acute peptic ulcer bleeding? A meta-analysis. Gastrointest Endosc. 2012; 76:283–292.24. Mochizuki S, Uedo N, Oda I, et al. Scheduled second-look endoscopy is not recommended after endoscopic submucosal dissection for gastric neoplasms (the SAFE trial): a multicentre prospective randomised controlled non-inferiority trial. Gut. 2015; 64:397–405.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Routine Second-Look Endoscopy Necessary for All Bleeding Peptic Ulcers?
- Short-Term Healing Process of Artificial Ulcers after Gastric Endoscopic Submucosal Dissection
- Is the Reinitiation of Antiplatelet Agents Safe at 1 Week after Gastric Endoscopic Submucosal Dissection? Assessment of Bleeding Risk Using the Forrest Classification
- Clinical Usefulness of Rockall Scoring System in Patients with Bleeding Peptic Ulcer-Comparison with Forrest Classification
- Usefulness of Narrow-Band Imaging in Endoscopic Submucosal Dissection of the Stomach