Int J Thyroidol.
2016 May;9(1):35-38. 10.11106/ijt.2016.9.1.35.
Surgical Technique for the Functional Preservation of the Inferior Parathyroid Glands
- Affiliations
-
- 1Department of Otorhinolaryngology, Bundang Jesaeng Hospital, Deajin Medical Center, Seongnam, Korea.
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Pusan National University School of Medicine and Biomedical Research Institute, Pusan National University, Busan, Korea. voiceleebj@gmail.com
- KMID: 2164914
- DOI: http://doi.org/10.11106/ijt.2016.9.1.35
Abstract
- BACKGROUND AND OBJECTIVES
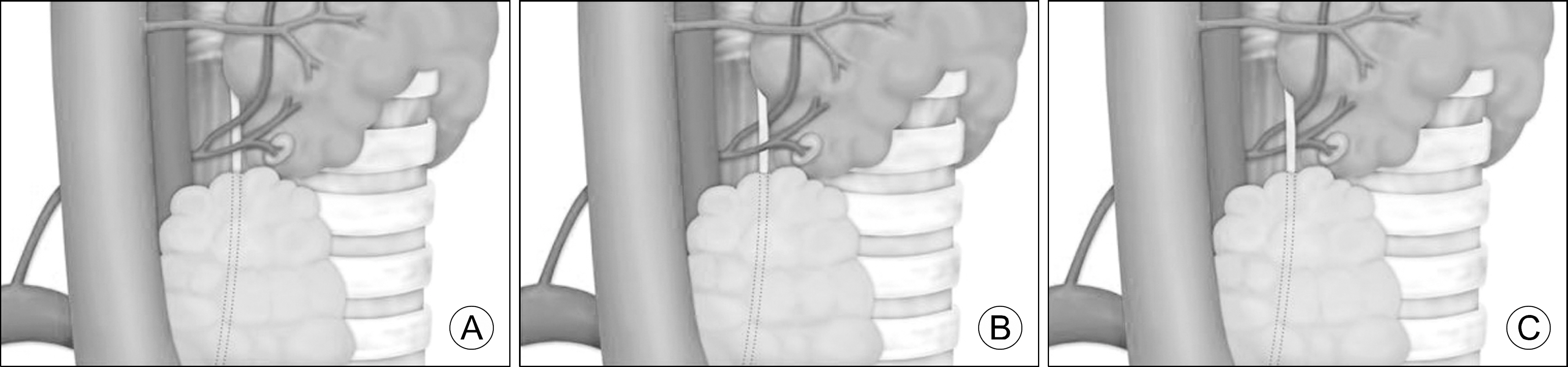
The inferior parathyroid glands receive their blood supply from the inferior thyroid artery. The anatomic relationship of this artery and the recurrent laryngeal nerve can assume three different patterns. To maintain the vascular supply of the inferior parathyroid glands during central neck dissection, we considered the anatomic relationship of these structures in our surgical approach.
MATERIALS AND METHODS
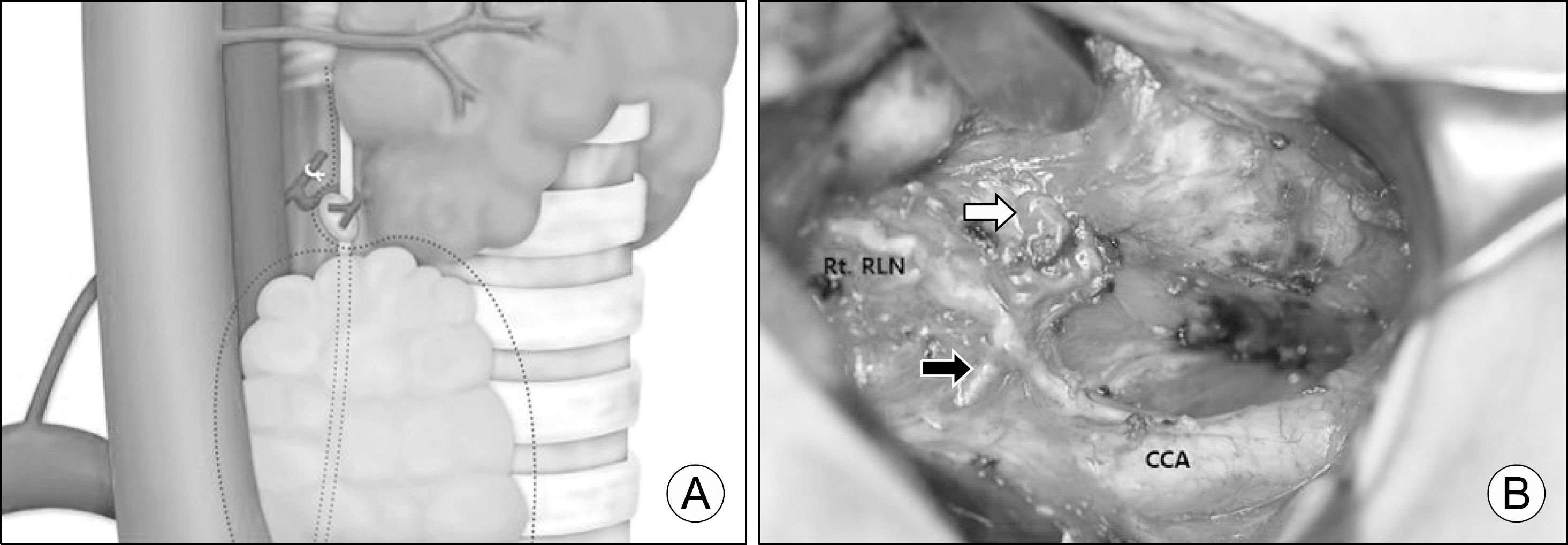
Fibrofatty tissue in the central neck compartment was removed by dissection proceeding along the recurrent laryngeal nerve. During the dissection, care was taken not to injure the vascular supply of the inferior parathyroid gland.
RESULTS
For an inferior parathyroid gland that receives its blood supply from the posterolateral vascular pedicle, preservation is achieved by performing the dissection along the recurrence laryngeal nerve on the gland's medial side. In patients in whom the inferior thyroid artery travels deep to the right recurrent laryngeal nerve, such that the right parathyroid gland receives its blood supply from the posteromedial vascular pedicle, central neck dissection should be performed carefully along the lateral side of the gland to preserve the pedicle.
CONCLUSION
Preservation of inferior parathyroid gland function requires a detailed understanding of the anatomic relationship between the inferior thyroid artery and recurrent laryngeal nerve. The direction of the dissection along the nerve should be adjusted according to its anatomic relationship to the inferior thyroid artery.
MeSH Terms
Figure
Reference
-
References
1. Moo TA, McGill J, Allendorf J, Lee J, Fahey T 3rd, Zarnegar R. Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg. 2010; 34(6):1187–91.
Article2. Bonnet S, Hartl D, Leboulleux S, Baudin E, Lumbroso JD, Al Ghuzlan A, et al. Prophylactic lymph node dissection for papillary thyroid cancer less than 2 cm: implications for radioiodine treatment. J Clin Endocrinol Metab. 2009; 94(4):1162–7.
Article3. Hughes DT, Doherty GM. Central neck dissection for papillary thyroid cancer. Cancer Control. 2011; 18(2):83–8.
Article4. Shen WT, Ogawa L, Ruan D, Suh I, Kebebew E, Duh QY, et al. Central neck lymph node dissection for papillary thyroid cancer: comparison of complication and recurrence rates in 295 initial dissections and reoperations. Arch Surg. 2010; 145(3):272–5.5. Lee DY, Cha W, Jeong WJ, Ahn SH. Preservation of the inferior thyroidal vein reduces post-thyroidectomy hypocalcemia. Laryngoscope. 2014; 124(5):1272–7.
Article6. Giordano D, Valcavi R, Thompson GB, Pedroni C, Renna L, Gradoni P, et al. Complications of central neck dissection in patients with papillary thyroid carcinoma: results of a study on 1087 patients and review of the literature. Thyroid. 2012; 22(9):911–7.
Article7. Sakorafas GH, Stafyla V, Bramis C, Kotsifopoulos N, Kolettis T, Kassaras G. Incidental parathyroidectomy during thyroid surgery: an underappreciated complication of thyroidectomy. World J Surg. 2005; 29(12):1539–43.
Article8. Abboud B, Sleilaty G, Braidy C, Zeineddine S, Ghorra C, Abadjian G, et al. Careful examination of thyroid specimen intraoperatively to reduce incidence of inadvertent parathyroidectomy during thyroid surgery. Arch Otolaryngol Head Neck Surg. 2007; 133(11):1105–10.
Article9. Sasson AR, Pingpank JF Jr, Wetherington RW, Hanlon AL, Ridge JA. Incidental parathyroidectomy during thyroid surgery does not cause transient symptomatic hypocalcemia. Arch Otolaryngol Head Neck Surg. 2001; 127(3):304–8.
Article10. Sheahan P, Mehanna R, Basheeth N, Murphy MS. Is systematic identification of all four parathyroid glands necessary during total thyroidectomy?: a prospective study. Laryngoscope. 2013; 123(9):2324–8.
Article11. Bliss RD, Gauger PG, Delbridge LW. Surgeon's approach to the thyroid gland: surgical anatomy and the importance of technique. World J Surg. 2000; 24(8):891–7.
Article12. Cocchiara G, Cajozzo M, Amato G, Mularo A, Agrusa A, Romano G. Terminal ligature of inferior thyroid artery branches during total thyroidectomy for multinodular goiter is associated with higher postoperative calcium and PTH levels. J Visc Surg. 2010; 147(5):e329–32.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Preservation of Parathyroid Glands during Thyroid Surgery
- Parathyroid Glands Location, vascular supply and preservation during a total thyroidectomy
- Near Infrared Autofluoroscence (NIRAF) in Thyroid Surgery
- Tips for Preservation of Parathyroid Gland During Thyroid Surgery
- Identification of Intrathyroidal Parathyroid Gland Using Near-Infrared Autofluorescence and Autotransplantation: Report of Two Cases