Ann Surg Treat Res.
2016 Jun;90(6):297-302. 10.4174/astr.2016.90.6.297.
An online questionnaire survey on preferred timing for the diagnosis and management of thyroid carcinoma in general population in Korea
- Affiliations
-
- 1Department of Surgery, College of Medicine Chungbuk National University, Cheongju, Korea. webjwpark@chungbuk.ac.kr
- 2Department of Surgery, Chungbuk National University Hospital, Cheongju, Korea.
- 3Department of Information & Communication Engineering, College of Electrical and Computer Engineering, Chungbuk National University, Cheongju, Korea.
- KMID: 2164789
- DOI: http://doi.org/10.4174/astr.2016.90.6.297
Abstract
- PURPOSE
An optimal timing for diagnosis and management of papillary thyroid microcarcinoma (PTMC) has become the subject for much controversy. The aim of the present study is to analyze people's preference in Korea for timing of diagnosis and management of PTMC using an online questionnaire.
METHODS
The questionnaire consists of 3 questions about preference for the diagnosis and management of PTMC and 3 additional questions about respondents' personal information. An online survey was conducted from March 3 to June 3 in 2015 using Google Survey (http://goo.gl/forms/b81yEjqNUA).
RESULTS
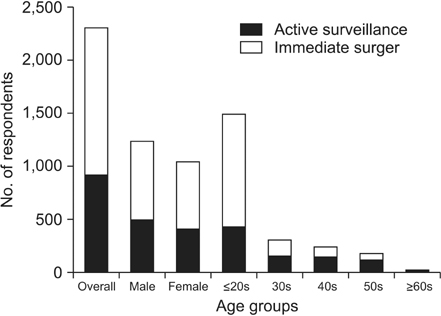
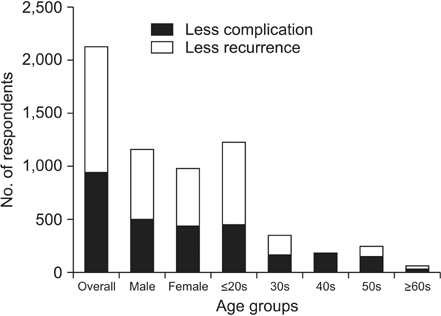
A total 2,308 persons (1,246 males, 1,053 females) answered the questionnaire. Respondents' ages varied widely from teenagers to 70-year-olds. If there was a suspicious thyroid nodule from PTMC measuring less than 1 cm in diameter, 95.7% of respondents want to know a cytological diagnosis for it. If a thyroid nodule turned out to be a PTMC, 59.5% of respondents wanted it removed immediately. For surgical management of PTMC, 53.0% of respondents were worried more about recurrences than complications. In subgroup analyses, respondents younger than 40 years old more often want immediate surgery than others: 66.7% vs. 32.7% (P < 0.05). Respondents who underwent thyroid cancer surgery (n = 91) were worried more about recurrences than others: 69.2% vs. 52.4% (P < 0.05).
CONCLUSION
Almost all respondents in the present study wanted diagnosis of suspicious thyroid nodules immediately. However, there were opposing opinions about the preferred timing for surgical treatment and surgical extents. A patient's right to know their disease status and decision on treatments should be emphasized all the more.
Keyword
MeSH Terms
Figure
Reference
-
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26:1–133.2. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN Guidelines): Thyroid carcinoma ver. 2 [Internet]. Fort Wathington (PA): National Comprehensive Cancer Network;c2015. cited 2016 Jan 19. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.3. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 2014; 81:Suppl 1. 1–122.4. Dralle H, Musholt TJ, Schabram J, Steinmüller T, Frilling A, Simon D, et al. German Association of Endocrine Surgeons practice guideline for the surgical management of malignant thyroid tumors. Langenbecks Arch Surg. 2013; 398:347–375.5. Brito JP, Morris JC, Montori VM. Thyroid cancer: zealous imaging has increased detection and treatment of low risk tumours. BMJ. 2013; 347:f4706.6. Yu XM, Wan Y, Sippel RS, Chen H. Should all papillary thyroid microcarcinomas be aggressively treated? An analysis of 18,445 cases. Ann Surg. 2011; 254:653–660.7. Wang TS, Goffredo P, Sosa JA, Roman SA. Papillary thyroid microcarcinoma: an over-treated malignancy? World J Surg. 2014; 38:2297–2303.8. Hay ID, Hutchinson ME, Gonzalez-Losada T, McIver B, Reinalda ME, Grant CS, et al. Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery. 2008; 144:980–987.9. Noguchi S, Yamashita H, Uchino S, Watanabe S. Papillary microcarcinoma. World J Surg. 2008; 32:747–753.10. Shrestha M, Crothers BA, Burch HB. The impact of thyroid nodule size on the risk of malignancy and accuracy of fine-needle aspiration: a 10-year study from a single institution. Thyroid. 2012; 22:1251–1256.11. McHenry CR, Huh ES, Machekano RN. Is nodule size an independent predictor of thyroid malignancy? Surgery. 2008; 144:1062–1068.12. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedus L, et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and EuropeanThyroid Association Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules. Endocr Pract. 2010; 16:Suppl 1. 1–43.13. Ito Y, Miyauchi A, Inoue H, Fukushima M, Kihara M, Higashiyama T, et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg. 2010; 34:28–35.14. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014; 24:27–34.15. Machens A, Holzhausen HJ, Dralle H. The prognostic value of primary tumor size in papillary and follicular thyroid carcinoma. Cancer. 2005; 103:2269–2273.16. Ito Y, Miyauchi A. Nonoperative management of low-risk differentiated thyroid carcinoma. Curr Opin Oncol. 2015; 27:15–20.17. Ito Y, Oda H, Miyauchi A. Insights and clinical questions about the active surveillance of low-risk papillary thyroid microcarcinomas. Endocr J. 2016; 63:323–328.18. Nilubol N, Kebebew E. Should small papillary thyroid cancer be observed? A population-based study. Cancer. 2015; 121:1017–1024.19. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006; 16:109–142.20. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.21. Kandil E, Noureldine SI, Abbas A, Tufano RP. The impact of surgical volume on patient outcomes following thyroid surgery. Surgery. 2013; 154:1346–1352.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Optimal Timing for Surgery in Well-differentiated Thyroid Carcinoma Detected during Pregnancy
- Successful Treatment of Cavernous Sinus Metastasis from Follicular Thyroid Carcinoma with Lenvatinib
- Management of Thyroid Nodules and Cancers Arising in the Elderly
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- A Case of Window Resection and Secondary Reconstruction of the Trachea Invaded by Papillary Thyroid Carcinoma