Pediatr Infect Vaccine.
2016 Apr;23(1):46-53. 10.14776/piv.2016.23.1.46.
Epidemiology and Clinical manifestations of Enterovirus in Pediatric Inpatient in Incheon
- Affiliations
-
- 1Department of Pediatrics, Inha University School of Medicine, Incheon, Korea. md21@inha.edu
- 2Incheon Research Institute of Public Health and Environment, Korea.
- KMID: 2163223
- DOI: http://doi.org/10.14776/piv.2016.23.1.46
Abstract
- PURPOSE
Enterovirus (EV) infection in children can manifest various diseases from asymptomatic infection to nonspecific febrile illness, hand-foot-mouth disease, and aseptic meningitis. This study was aimed to investigate epidemiology and clinical significance of various genotypes of EV infections in pediatric inpatient.
METHODS
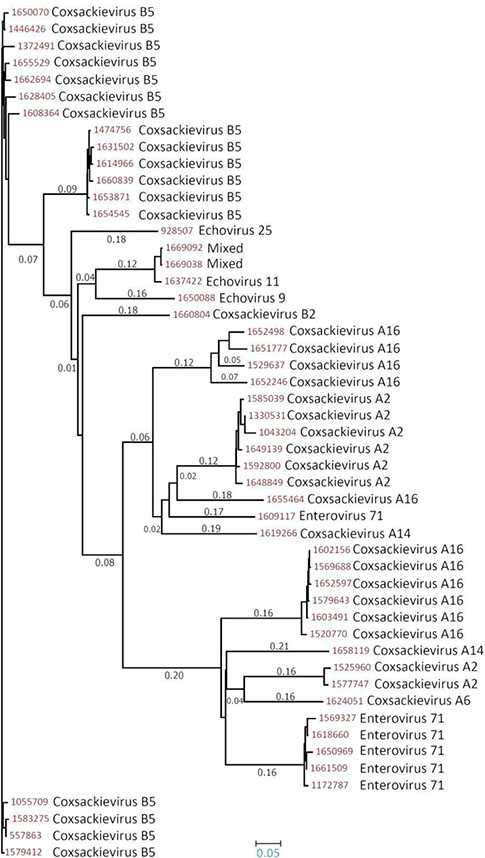
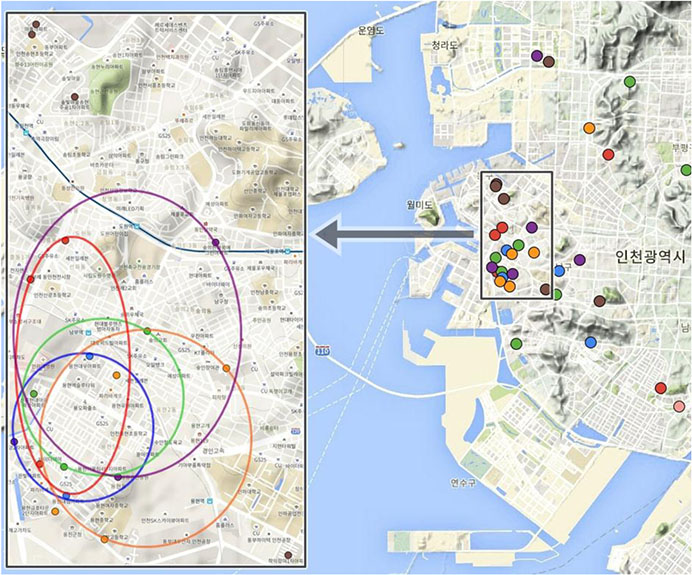
We collected the stool samples from the admitted pediatric patients in Inha University Hospital from March 2014 to March 2015. EV detection and genotype identification were performed by real-time RT-PCR and semi-nested RT-PCR. Phylogenetic trees were constructed by neighbor joining method.
RESULTS
A total of 400 samples were collected during study period and 112 patients (28%) were diagnosed with EV infections. The mean age of EV positive patients was 2.66 years (0.1-14) and sex ratio was 1.73:1. Genetic sequences of EVs were identified; coxsackievirus B5 (17, 15.2%), coxsackievirus A16 (13, 11.6%), enterovirus 71 (10, 8.9%), and coxsackievirus A2 (9, 8.0%). Nonspecific febrile illness (96, 86%) was the most common clinical manifestation and the duration of fever was 0-11 days (mean 3.1 days). Rash (44, 39%) and meningitis (43, 38%) were followed. Patients who were attending daycare center or had siblings accounted for 82.1%. Phylogenetic relationship tree revealed 6 distinct genogroups among 56 types of EVs.
CONCLUSIONS
This study is the report of epidemiology, serotype distribution and clinical manifestations of children with EV infection in Incheon. This data will be helpful for further study about the epidemiology of EV infection in Korea.
Keyword
MeSH Terms
Figure
Reference
-
1. Abzug MJ. Nonpolio enteroviruses. In : Kliegman RM, Stanton BF, Schor NF, Geme JWS, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Elsevier saunders;2011. p. 1088–1094.2. Park KS, Choi YJ, Park JS. Enterovirus infection in Korean children and antienteroviral potential candidate agent. Korean J Pediatr. 2012; 55:359–366.
Article3. Modlin JF. Enteroviruses and parechoviruses. In : Long SS, Pickering LK, Prober CG, editors. Principles and practice of pediatric infectious diseases. 4th ed. Philadelphia: Elsevier saunders;2012. p. 1172–1179.4. Jee YM, Cheon DS, Choi WY, Ahn JB, Kim KS, Chung YS, et al. Updates on enterovirus surveillance in Korea. Infect Chemother. 2004; 36:294–303.5. Wu Y, Yeo A, Phoon MC, Tan EL, Poh CL, Quak SH, et al. The largest outbreak of hand; foot and mouth disease in Singapore in 2008: the role of enterovirus 71 and coxsackievirus A strains. Int J Infect Dis. 2010; 14:e1076–e1081.
Article6. Yang F, Ren L, Xiong Z, Li J, Xiao Y, Zhao R, et al. Enterovirus 71 outbreak in the People's Republic of China in 2008. J Clin Microbiol. 2009; 47:2351–2352.
Article7. Fujimoto T, Iizuka S, Enomoto M, Abe K, Yamashita K, et al. Hand, foot, and mouth disease caused by coxsackievirus A6, Japan, 2011. Emerg Infect Dis. 18:337–339.
Article8. Infectious Disease Surveillance Center. Virus isolation/detection from hand, foot and mouth disease cases, 2007-2011. Infectious Agents Surveillance Report. 24 September 2015. Available at: http:// idsc.nih.go.jp/iasr/prompt/s2graph-pke.html.9. Puenpa J, Mauleekoonphairoj J, Linsuwanon P, Suwannakarn K, Chieochansin T, Korkong S, et al. Prevalence and characterization of enterovirus infections among pediatric patients with hand foot mouth disease, herpangina and influenza like illness in Thailand, 2012. PLoS One. 2014; 9:e98888.
Article10. Korea Centers. National laboratory surveillance for enterovirus. Public Health Wkly Rep. 2008; 1:617–621.11. Baek KA, Yeo SG, Lee BH, Park KS, Song JH, Yu JS, et al. Epidemics of enterovirus infection in Chungnam Korea, 2008 and 2009. Virology Journal. 2011; 8:297.
Article12. Park KS, Lee BH, Baek KA, Cheon DS, Yeo SG, Park JS, et al. Enteroviruses isolated from herpangina and hand-foot-andmouth disease in Korean children. Virology Journal. 2012; 9:205.
Article13. Park KS, Choi YJ, Park JS. Enterovirus infection in Korean children and antienteroviral potential candidate agent. Korean J Pediatr. 2012; 55:359–366.
Article14. Seo JH, Yeom JS, Youn HS, Han TH, Chung JY. Prevalence of human parechovirus and enterovirus in cerebrospinal fluid samples in children in Jinju, Korea. Korean J Pediatr. 2015; 58:102–107.
Article15. Park IS, Lee HS, Choi SH, Kim HJ, Hwang SY, Cheon DS, et al. Epidemiology and clinical characteristics of enterovirus infections in children: a single center analysis from 2006 to 2010. Korean J Pediatr Infect Dis. 2013; 20:81–88.
Article16. Baek DW, Kim JM, Kim KH, Ahn JG, Kim DS. Epidemiologic and clinical features of enteroviral infections in children, a single center study in Korea: 2009. Korean J Pediatr Infect Dis. 2010; 17:122–129.
Article17. Pöyry T, Kinnunen L, Hyypiä T, Brown B, Horsnell C, Hovi T, et al. Genetic and phylogenetic clustering of enteroviruses. J Gen Virol. 1996; 77:1699–1717.
Article18. Ragonnet-Cronin M, Hodcroft E, Hué S, Fearnhill E, Delpech V, Brown AJ, et al. Automated analysis of phylogenetic clusters. BMC Bioinformatics. 2013; 14:317.
Article19. Rosychuk RJ. Identifying geographic areas with high disease rates: when do confidence intervals for rates and a disease cluster detection method agree. Int J Health Geogr. 2006; 5:46.20. Li W, Zhang X, Chen X, Cheng YP, Wu YD, Shu Q, et al. Epidemiology of childhood enterovirus infections in Hangzhou, China. Virol J. 2015; 12:58.
Article21. Jeon JS, Kim JK, Yu JS, Kim JW. Epidemic trends of enterovirus infections from pediatric patients in Cheonan, Korea. J Clin Lab Anal. 2016; 30:161–164.
Article23. Witsø E, Cinek O, Aldrin M, Grinde B, Rasmussen T, Wetlesen T, et al. Predictors of sub-clinical enterovirus infections in infants: a prospective cohort study. Int J Epidemiol. 2010; 39:459–468.
Article24. Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987; 4:406–425.25. Zhang S, Zhao J. Spatio-temporal epidemiology of hand, foot and mouth disease in Liaocheng City, North China. Exp Ther Med. 2015; 9:811–816.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurologic Manifestations according to Serotypes of Enterovirus in Pediatric Inpatient in Incheon
- Epidemiology of the Enterovirus in Korea
- Enterovirus Infection in Adults Presenting with Nonspecific Febrile Illness during Summer
- Epidemiology and Clinical Characteristics of Enterovirus Infections in Children: A Single Center Analysis from 2006 to 2010
- Neurological Manifestations and Experience with IV Immunoglobulin in Children with Enterovirus 71 Infections