Ann Surg Treat Res.
2016 May;90(5):257-264. 10.4174/astr.2016.90.5.257.
Risk factors for cancer recurrence or death within 6 months after liver resection in patients with colorectal cancer liver metastasis
- Affiliations
-
- 1Division of HBP Surgery and Liver Transplantation, Department of Surgery, Korea University College of Medicine, Seoul, Korea. kimds1@korea.ac.kr
- KMID: 2163065
- DOI: http://doi.org/10.4174/astr.2016.90.5.257
Abstract
- PURPOSE
The aim of this study was to find risk factors for early recurrence (ER) and early death (ED) after liver resection for colorectal cancer liver metastasis (CRCLM).
METHODS
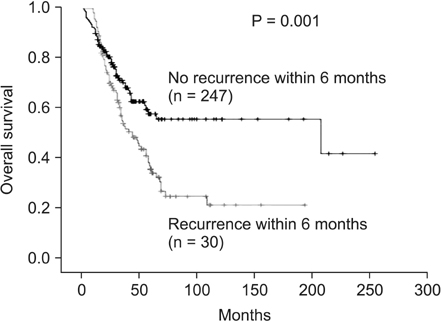
Between May 1990 and December 2011, 279 patients underwent liver resection for CRCLM at Korea University Medical Center. They were assigned to group ER (recurrence within 6 months after liver resection) or group NER (non-ER; no recurrence within 6 months after liver resection) and group ED (death within 6 months after liver resection) or group NED (alive > 6 months after liver resection).
RESULTS
The ER group included 30 patients (10.8%) and the NER group included 247 patients (89.2%). The ED group included 18 patients (6.6%) and the NED group included 253 patients (93.4%). Prognostic factors for ER in a univariate analysis were poorly differentiated colorectal cancer (CRC), synchronous metastasis, ≥5 cm of liver mass, ≥50 ng/mL preoperative carcinoembryonic antigen level, positive liver resection margin, and surgery alone without perioperative chemotherapy. Prognostic factors for ED in a univariate analysis were poorly differentiated CRC, positive liver resection margin, and surgery alone without perioperative chemotherapy. Multivariate analysis showed that poorly differentiated CRC, ≥5-cm metastatic tumor size, positive liver resection margin, and surgery alone without perioperative chemotherapy were independent risk factors related to ER. For ED, poorly differentiated CRC, positive liver resection margin, and surgery alone without perioperative chemotherapy were risk factors in multivariate analysis.
CONCLUSION
Complete liver resection with clear resection margin and perioperative chemotherapy should be carefully considered when patients have the following preoperative risk factors: metastatic tumor size ≥ 5 cm and poorly differentiated CRC.
MeSH Terms
Figure
Cited by 1 articles
-
Hepatic resection after neoadjuvant chemotherapy for patients with liver metastases from colorectal cancer: need for cautious planning
Young Il Kim, In Ja Park, Jeong Eun Kim, So Yeon Kim, Jin-Hong Park, Jae Hoon Lee, Tae Yong Ha, Yong Sang Hong, Sun Young Kim, Tae Won Kim, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Ann Surg Treat Res. 2019;97(5):245-253. doi: 10.4174/astr.2019.97.5.245.
Reference
-
1. Adam R, De Gramont A, Figueras J, Guthrie A, Kokudo N, Kunstlinger F, et al. The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist. 2012; 17:1225–1239.2. de Jong MC, Pulitano C, Ribero D, Strub J, Mentha G, Schulick RD, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009; 250:440–448.3. Fortner JG. Recurrence of colorectal cancer after hepatic resection. Am J Surg. 1988; 155:378–382.4. Takahashi S, Konishi M, Nakagohri T, Gotohda N, Saito N, Kinoshita T. Short time to recurrence after hepatic resection correlates with poor prognosis in colorectal hepatic metastasis. Jpn J Clin Oncol. 2006; 36:368–375.5. Choti MA, Sitzmann JV, Tiburi MF, Sumetchotimetha W, Rangsin R, Schulick RD, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg. 2002; 235:759–766.6. Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999; 230:309–318.7. Vigano L, Capussotti L, Lapointe R, Barroso E, Hubert C, Giuliante F, et al. Early recurrence after liver resection for colorectal metastases: risk factors, prognosis, and treatment. A LiverMetSurvey-based study of 6,025 patients. Ann Surg Oncol. 2014; 21:1276–1286.8. Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg. 1995; 19:59–71.9. Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005; 241:715–722.10. Turrini O, Viret F, Guiramand J, Lelong B, Bege T, Delpero JR. Strategies for the treatment of synchronous liver metastasis. Eur J Surg Oncol. 2007; 33:735–740.11. Koga H, Moriya Y, Akasu T, Fujita S. The relationship between prognosis and CEAdt after hepatic resection in patients with colorectal carcinomas. Eur J Surg Oncol. 1999; 25:292–296.12. Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trial. Lancet. 2008; 371:1007–1016.13. Meyerhardt JA, Mayer RJ. Systemic therapy for colorectal cancer. N Engl J Med. 2005; 352:476–487.14. Leonard GD, Brenner B, Kemeny NE. Neoadjuvant chemotherapy before liver resection for patients with unresectable liver metastases from colorectal carcinoma. J Clin Oncol. 2005; 23:2038–2048.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver Metastases in Colorectal Cancer
- Risk Stratification of T1 Colorectal Cancer Metastasis to Lymph Nodes: Current Status and Perspective
- Outcomes of a Hepatic Resection for Colorectal-Carcinoma Liver Metastases
- Adjuvant oxaliplatin-based chemotherapy effect after treatment of colorectal hepatic metastasis
- Pattern of Recurrences and Metastases after a Curative Resection for Primary Colorectal Cancer