Korean J Neurotrauma.
2016 Apr;12(1):6-10. 10.13004/kjnt.2016.12.1.6.
Symptomatic Epidural Fluid Collection Following Cranioplasty after Decompressive Craniectomy for Traumatic Brain Injury
- Affiliations
-
- 1Department of Neurosurgery, College of Medicine, Chosun University, Gwangju, Korea. ns64902@hanmail.net
- KMID: 2163008
- DOI: http://doi.org/10.13004/kjnt.2016.12.1.6
Abstract
OBJECTIVE
Symptomatic epidural fluid collection (EFC) arising as a complication of cranioplasty is underestimated and poorly described. The purpose of this study was to investigate the risk factors for development of symptomatic EFC after cranioplasty following traumatic brain injury (TBI).
METHODS
From January 2010 to December 2014, 82 cranioplasties following decompressive hemicraniectomy for TBI were performed by a single surgeon. Of these 82 patients, 17 were excluded from this study due to complications including postoperative hematoma, hydrocephalus, or infection. Sixty-five patients were divided into 2 groups based on whether they had developed symptomatic EFC: 13 patients required an evacuation operation due to symptomatic EFC after cranioplasty (Group I), and 52 obtained good outcome without development of symptomatic EFC (Group II). We compared the 2 groups to identify the risk factors for symptomatic EFC according to sex, age, initial diagnosis, timing of cranioplasty, cerebrospinal fluid (CSF) leakage during cranioplasty, size of bone flap, and bone material.
RESULTS
A large bone flap and CSF leakage during cranioplasty were identified as the statistically significant risk factors (p<0.05) for development of symptomatic EFC. In Group I, 11 patients were treated successfully with 5 L catheter drainage, but 2 patients showed recurrent EFC, eventually necessitating bone flap removal.
CONCLUSION
A larger skull defect and intraoperative CSF leakage are proposed to be the significant risk factors for development of symptomatic EFC. Careful attention to avoid CSF leakage during cranioplasty is needed to minimize the occurrence of EFC, especially in cases featuring a large cranial defect.
MeSH Terms
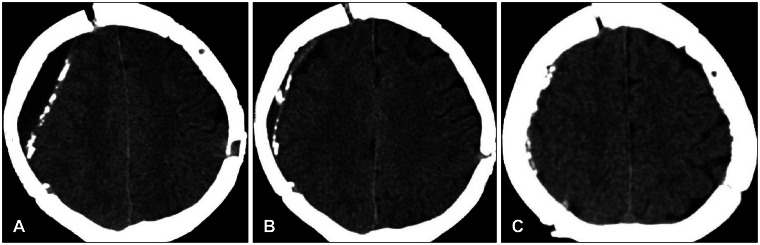
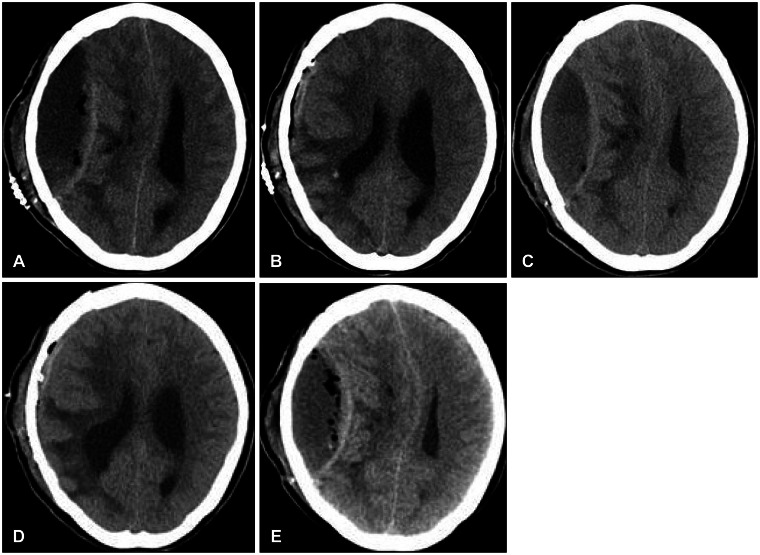
Figure
Reference
-
1. Aarabi B, Hesdorffer DC, Ahn ES, Aresco C, Scalea TM, Eisenberg HM. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006; 104:469–479. PMID: 16619648.
Article2. Aoki N. Air in acute epidural hematomas. Report of two cases. J Neurosurg. 1986; 65:555–556. PMID: 3760966.3. Bobinski L, Koskinen LO, Lindvall P. Complications following cranioplasty using autologous bone or polymethylmethacrylate--retrospective experience from a single center. Clin Neurol Neurosurg. 2013; 115:1788–1791. PMID: 23725651.
Article4. Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D. Out-comes of cranial repair after craniectomy. J Neurosurg. 2010; 112:1120–1124. PMID: 19612971.
Article5. Cheng YK, Weng HH, Yang JT, Lee MH, Wang TC, Chang CN. Factors affecting graft infection after cranioplasty. J Clin Neurosci. 2008; 15:1115–1119. PMID: 18656363.
Article6. Coulter IC, Pesic-Smith JD, Cato-Addison WB, Khan SA, Thompson D, Jenkins AJ, et al. Routine but risky: a multi-centre analysis of the outcomes of cranioplasty in the Northeast of England. Acta Neurochir (Wien). 2014; 156:1361–1368. PMID: 24752723.
Article7. Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 2009; 26:E9. PMID: 19485722.
Article8. Kim JS, Cheong JH, Ryu JI, Kim JM, Kim CH. Bone flap resorption following cranioplasty after decompressive craniectomy: preliminary report. Korean J Neurotrauma. 2015; 11:1–5. PMID: 27169057.
Article9. Lee JW, Kim JH, Kang HI, Moon BG, Lee SJ, Kim JS. Epidural fluid collection after cranioplasty: fate and predictive factors. J Korean Neurosurg Soc. 2011; 50:231–234. PMID: 22102954.10. Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V. Clinical outcome in cranioplasty: critical review in long-term follow-up. J Craniofac Surg. 2003; 14:144–153. PMID: 12621283.
Article11. Park JS, Lee KS, Shim JJ, Yoon SM, Choi WR, Doh JW. Large defect may cause infectious complications in cranioplasty. J Korean Neurosurg Soc. 2007; 42:89–91.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Reappraisal of the Necessity of a Ventriculoperitoneal Shunt After Decompressive Craniectomy in Traumatic Brain Injury
- Paradoxical Herniation after Decompressive Craniectomy for Acute Subdural Hematoma
- Pushed-out Scrylic Bone Flap n Post-traumatic Hydrocephalus
- Safety and Efficacy of Early Cranioplasty after Decompressive Craniectomy in Traumatic Brain Injury Patients
- Epidural Fluid Collection after Cranioplasty : Fate and Predictive Factors