Investig Magn Reson Imaging.
2016 Mar;20(1):61-65. 10.13104/imri.2016.20.1.61.
Subperiosteal Osteoid Osteoma of the Knee: Case Report
- Affiliations
-
- 1Department of Radiology, Pusan National University Hospital, Biomedical Research Institute, Busan, Korea. lis@pusan.ac.kr
- 2Pusan National University School of Medicine, Busan, Korea.
- 3Department of Orthopaedic Surgery, Pusan National University Hospital, Biomedical Research Institute, Busan, Korea.
- 4Department of Radiology, Inje University Haeundae Paik Hospital, Busan, Korea.
- KMID: 2161371
- DOI: http://doi.org/10.13104/imri.2016.20.1.61
Abstract
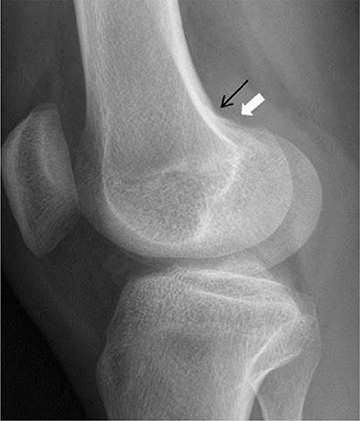
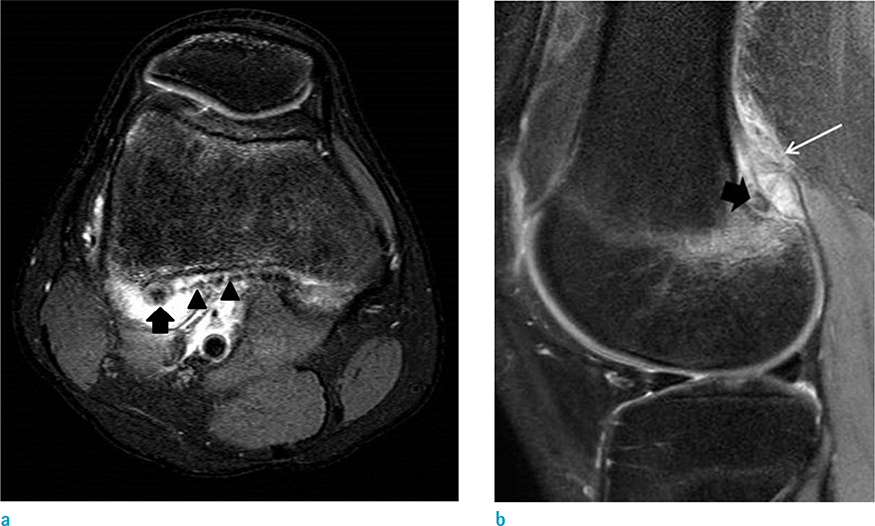
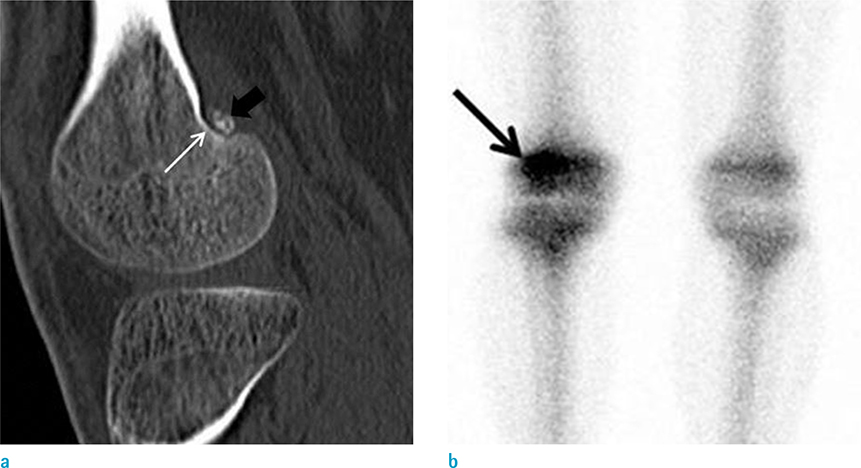
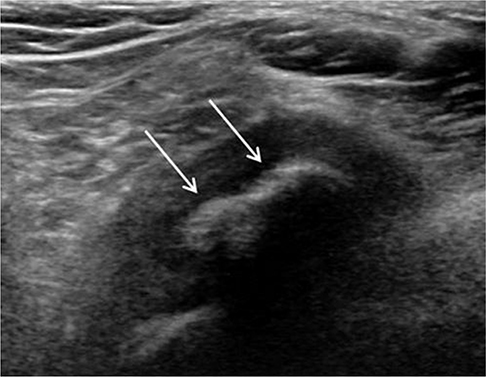
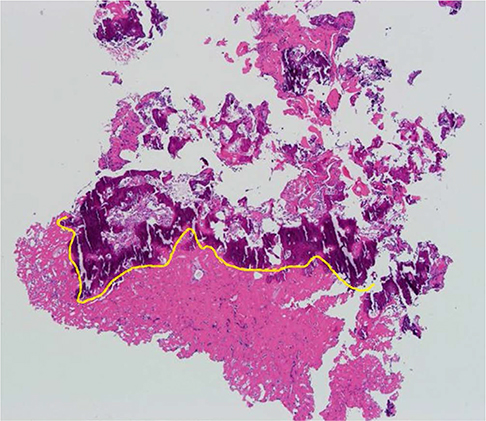
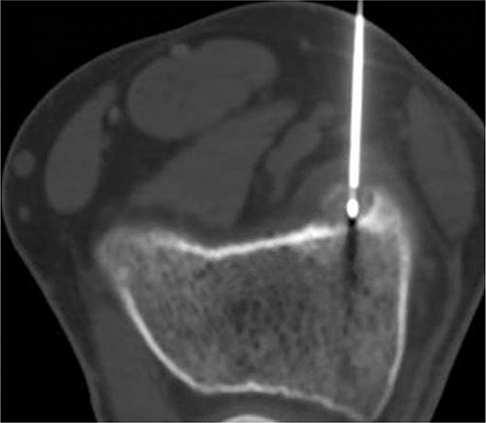
- Osteoid osteoma, a frequent lesions of bone, is usually intraosseous but occasionally subperiosteal. We describe the case of a 19-year-old male with knee pain caused by subperiosteal osteoid osteoma. Radiologic evaluation was performed with radiographic, computed tomography (CT), ultrasonographic (US) and magnetic resonance imaging (MRI). But the preoperative diagnosis of osteoid osteoma was delayed because of unusual imaging findings and atypical symptom. After excisional biopsy, histological examination confirmed the diagnosis of osteoid osteoma. The lesion was treated successfully with CT-guided radiofrequency ablation.
Keyword
MeSH Terms
Figure
Reference
-
1. Suresh SS, Rani V. Atypical periosteal osteoid osteoma: a case report. Cases J. 2009; 2:124.2. Kayser F, Resnick D, Haghighi P, et al. Evidence of the subperiosteal origin of osteoid osteomas in tubular bones: analysis by CT and MR imaging. AJR Am J Roentgenol. 1998; 170:609–614.3. Khan JA, Vaidya S, Devkota P, Acharya BM, Pradhan NM, Shrestha S. Subperiosteal osteoid osteoma of the neck of talus. JNMA J Nepal Med Assoc. 2009; 48:58–61.4. Kitsoulis P, Mantellos G, Vlychou M. Osteoid osteoma. Acta Orthop Belg. 2006; 72:119–125.5. Motamedi D, Learch TJ, Ishimitsu DN, et al. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics. 2009; 29:2127–2141.6. Cakar M, Esenyel CZ, Seyran M, et al. Osteoid osteoma treated with radiofrequency ablation. Adv Orthop. 2015; 2015:807274.7. Chai JW, Hong SH, Choi JY, et al. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics. 2010; 30:737–749.