Ann Clin Microbiol.
2016 Mar;19(1):7-12. 10.5145/ACM.2016.19.1.7.
Increase of Clostridium difficile in Community; Another Worrisome Burden for Public Health
- Affiliations
-
- 1Department of Laboratory Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 2Department of Laboratory Medicine and Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea. hjkim12@yuhs.ac
- KMID: 2160079
- DOI: http://doi.org/10.5145/ACM.2016.19.1.7
Abstract
- BACKGROUND
Increasing rates of Clostridium difficile infection (CDI) have been reported mainly in Europe and North America; however, only limited reports have originated in Korea. The current epidemiology of CDI in the community could help to understand the outpatient healthcare environment and to extend infection control measures to outpatient settings.
METHODS
C. difficile isolates in NHIS Ilsan Hospital from 2012 to 2014 were included in this study. Clinical characteristics, acquisition types, and previous antimicrobial therapy were obtained via Electronic Medical Records. C. difficile culture was performed only in unformed stool. Toxin was positive by enzyme-linked fluorescent immunoassay (ELFA) in 247 specimens. In addition, toxin B and binary toxin gene were detected by PCR in 57 specimens. CDI was defined by toxigenic C. difficile isolation in unformed stool.
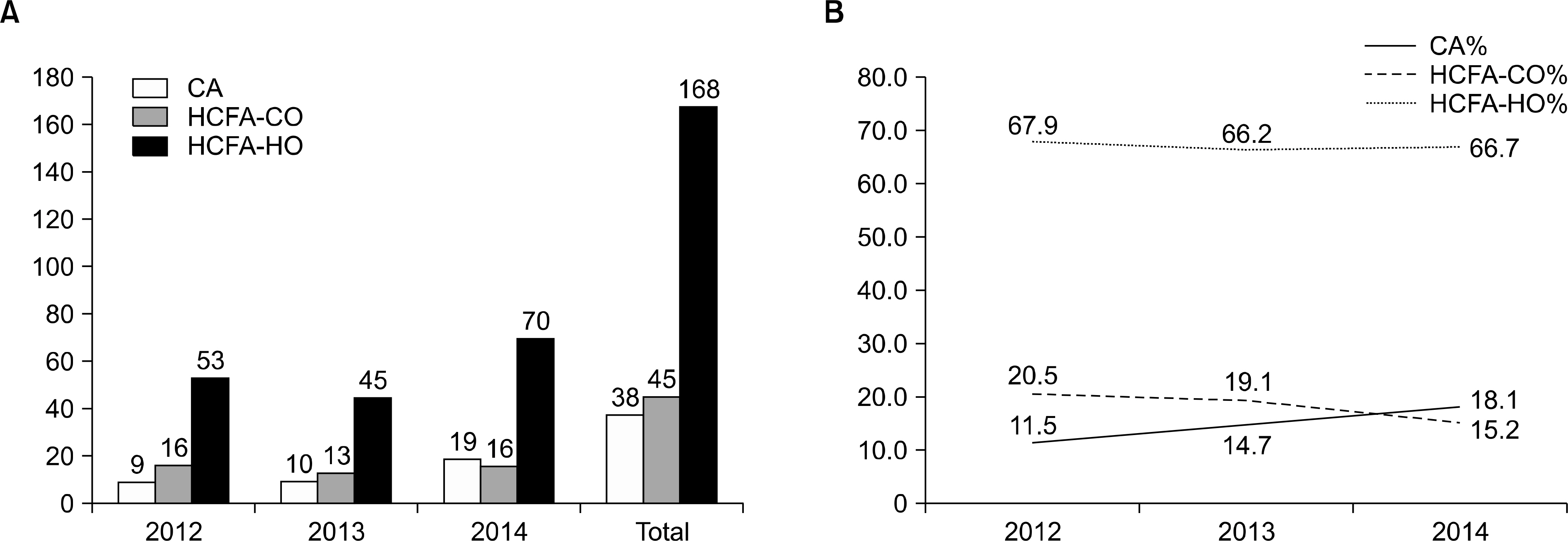
RESULTS
In the previous 3 years, 251 unduplicated C. difficile cases have been detected; 168 healthcare facility- associated hospital onset (HCFA-HO), 45 healthcare facility-associated community onset (HCFA-CO), and 38 community-associated (CA). Toxin positive rates by ELFA for toxin A&B were HCFA-HO 50.6% (84/166), HCFA-CO 41.9% (18/43), and CA 42.1% (16/38). Toxin positive rate by PCR for tcdB were HCFA-HO 62.9% (22/35), HCFA-CO 69.2% (9/13), and CA 100% (9/9). No binary toxin (cdtA/cdtB) was detected in 57 cases.
CONCLUSION
Community-associated CDI may be underestimated in Goyang province, Korea, especially by commonly used ELFA toxin assay. The spread of community-associated CDI should be recognized as an increasing burden of public health.
MeSH Terms
Figure
Cited by 1 articles
-
Analyzing Patterns for Stool Culture Requests by Physicians to Improve Quality
Hyoshim Shin, Sunjoo Kim
Lab Med Online. 2019;9(1):22-25. doi: 10.3343/lmo.2019.9.1.22.
Reference
-
References
1. Dubberke ER, Reske KA, Yan Y, Olsen MA, McDonald LC, Fraser VJ. Clostridium difficile–associated disease in a setting of endemicity: identification of novel risk factors. Clin Infect Dis. 2007; 45:1543–9.
Article2. Bignardi GE. Risk factors for Clostridium difficile infection. J Hosp Infect. 1998; 40:1–15.
Article3. Zilberberg MD, Shorr AF, Kollef MH. Increase in adult Clostridium difficile-related hospitalizations and case-fatality rate, United States, 2000–2005. Emerg Infect Dis. 2008; 14:929–31.4. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. http://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf. [Online] (last visited on 15 March 2016).5. Kim YS, Han DS, Kim YH, Kim WH, Kim JS, Kim HS, et al. Incidence and clinical features of Clostridium difficile infection in Korea: a nationwide study. Epidemiol Infect. 2013; 141:189–94.6. Tan XQ, Verrall AJ, Jureen R, Riley TV, Collins DA, Lin RT, et al. The emergence of community-onset Clostridium difficile infection in a tertiary hospital in Singapore: a cause for concern. Int J Antimicrob Agents. 2014; 43:47–51.
Article7. Chitnis AS, Holzbauer SM, Belflower RM, Winston LG, Bamberg WM, Lyons C, et al. Epidemiology of community-associated Clostridium difficile infection, 2009 through 2011. JAMA Intern Med. 2013; 173:1359–67.8. Gupta A and Khanna S. Community-acquired Clostridium difficile infection: an increasing public health threat. Infect Drug Resist. 2014; 7:63–72.9. Choi HK, Kim KH, Lee SH, Lee SJ. Risk factors for recurrence of Clostridium difficile infection: effect of vancomycin-resistant enterococci colonization. J Korean Med Sci. 2011; 26:859–64.10. Shin BM, Moon SJ, Kim YS, Shin WC, Yoo HM. Characterization of cases of Clostridium difficile infection (CDI) presenting at an emergency room: molecular and clinical features differentiate community-onset hospital-associated and community-associated CDI in a tertiary care hospital. J Clin Microbiol. 2011; 49:2161–5.
Article11. Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431–55.
Article12. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Health care–associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med. 2002; 137:791–7.
Article13. Dubberke ER, Carling P, Carrico R, Donskey CJ, Loo VG, McDonald LC, et al. Strategies to prevent Clostridium difficile infections in acute care hospitals: 2014 Update. Infect Control Hosp Epidemiol. 2014; 35:628–45.
Article14. Bacci S, Mølbak K, Kjeldsen MK, Olsen KE. Binary toxin and death after Clostridium difficile infection. Emerg Infect Dis. 2011; 17:976–82.15. Evans CT and Safdar N. Current trends in the epidemiology and outcomes of Clostridium difficile infection. Clin Infect Dis. 2015; 60(Suppl 2):S66–71.16. Ogielska M, Lanotte P, Le Brun C, Valentin AS, Garot D, Tellier AC, et al. Emergence of community-acquired Clostridium difficile infection: the experience of a French hospital and review of the literature. Int J Infect Dis. 2015; 37:36–41.
Article17. Mori N and Aoki Y. Clinical characteristics and risk factors for community-acquired Clostridium difficile infection: A retrospective, case-control study in a tertiary care hospital in Japan. J Infect Chemother. 2015; 21:864–7.18. Tan XQ, Verrall AJ, Jureen R, Riley TV, Collins DA, Lin RT, et al. The emergence of community-onset Clostridium difficile infection in a tertiary hospital in Singapore: a cause for concern. Int J Antimicrob Agents. 2014; 43:47–51.
Article19. Dantes R, Mu Y, Hicks LA, Cohen J, Bamberg W, Beldavs ZG, et al. Association between outpatient antibiotic prescribing practices and community-associated Clostridium difficile infection. Open Forum Infect Dis. 2015; 2:ofv113.
Article20. Clabots CR, Johnson S, Olson MM, Peterson LR, Gerding DN. Acquisition of Clostridium difficile by hospitalized patients: evidence for colonized new admissions as a source of infection. J Infect Dis. 1992; 166:561–7.
Article21. McFarland LV, Mulligan ME, Kwok RY, Stamm WE. Nosocomial acquisition of Clostridium difficile infection. N Engl J Med. 1989; 320:204–10.
Article22. Johnson S, Clabots CR, Linn FV, Olson MM, Peterson LR, Gerding DN. Nosocomial Clostridium difficile colonisation and disease. Lancet. 1990; 336:97–100.
Article23. Hung YP, Tsai PJ, Hung KH, Liu HC, Lee CI, Lin HJ, et al. Impact of toxigenic Clostridium difficile colonization and infection among hospitalized adults at a district hospital in southern Taiwan. PLoS One. 2012; 7:e42415.
Article24. Alcalá L, Reigadas E, Marín M, Martín A, Catalán P, Bouza E. Spanish Clostridium difficile Study Group. Impact of clinical awareness and diagnostic tests on the underdiagnosis of Clostridium difficile infection. Eur J Clin Microbiol Infect Dis. 2015; 34:1515–25.
Article25. Mohan SS, McDermott BP, Parchuri S, Cunha BA. Lack of value of repeat stool testing for Clostridium difficile toxin. Am J Med. 2006; 119:356. .e7–8.
Article26. Lo Vecchio A and Zacur GM. Clostridium difficile infection: an update on epidemiology, risk factors, and therapeutic options. Curr Opin Gastroenterol. 2012; 28:1–9.27. Maroo S and Lamont JT. Recurrent Clostridium difficile. Gastroenterology. 2006; 130:1311–6.
Article28. Gerding DN, Johnson S, Rupnik M, Aktories K. Clostridium difficile binary toxin CDT: mechanism, epidemiology, and potential clinical importance. Gut Microbes. 2014; 5:15–27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clostridium difficile Infection: What's New?
- Clostridium difficile Infection: A Worldwide Disease
- SDS-PAGE profiles of clostridium difficile isolated from patientsand hospital environments
- New Treatment Option for Recurrent Clostridium difficile Infection
- Determination of toxin production of clostridium difficile strains isolated from patients with suspected antibiotic associated diarrhea