Korean J Endocr Surg.
2016 Mar;16(1):6-12. 10.16956/kaes.2016.16.1.6.
Lateral Lymph Node Metastasis Prediction in Papillary Thyroid Cancer Patients with Suspicious Preoperative Imaging Findings
- Affiliations
-
- 1Department of Surgery, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- 2Department of Surgery, Gyeongsang National University Changwon Hospital, Gyeongsang National University School of Medicine, Changwon, Korea. drjej@gnu.ac.kr
- KMID: 2158622
- DOI: http://doi.org/10.16956/kaes.2016.16.1.6
Abstract
- PURPOSE
Lateral lymph node metastasis of papillary thyroid cancer (PTC) is indicative of tumor aggressiveness and can determine treatment strategies. However, the role of prophylactic lateral lymph node dissection in the management of PTC is unclear. This study evaluated factors predictive of lateral lymph node metastasis in patients with suspicious lymph node enlargement in preoperative imaging.
METHODS
This retrospective study included 728 patients with newly diagnosed PTC who underwent therapeutic surgery. Clinicopathologic results were reviewed, and factors predictive of lateral lymph node metastasis were analyzed.
RESULTS
Of the 242 patients with lymph node metastasis, 50 had lateral lymph node metastasis. Lateral lymph node metastasis was associated with sex, tumor size, preoperative thyroid stimulating hormone (TSH) concentration and presence of central lymph node metastasis. Among patients with suspicious lateral lymph node metastasis by ultrasonography, high TSH level (odds ratio 3.833, P=0.031) and number of metastatic central lymph nodes (odds ratio 3.68, P=0.025) were significantly predictive of lateral lymph node metastasis.
CONCLUSION
High serum TSH level and central lymph node metastasis were predictive of lateral lymph node metastasis in PTC patients with suspicious preoperative imaging findings. These predictive factors might help reduce unnecessary therapeutic lateral lymph node dissection.
MeSH Terms
Figure
Reference
-
References
1. Noguchi S, Noguchi A, Murakami N. Papillary carcinoma of the thyroid. I. Developing pattern of metastasis. Cancer. 1970; 26:1053–60.
Article2. Ito Y, Miyauchi A. Lateral lymph node dissection guided by preoperative and intraoperative findings in differentiated thyroid carcinoma. World J Surg. 2008; 32:729–39.
Article3. Ito Y, Jikuzono T, Higashiyama T, Asahi S, Tomoda C, Takamura Y, et al. Clinical significance of lymph node metastasis of thyroid papillary carcinoma located in one lobe. World J Surg. 2006; 30:1821–8.
Article4. Noguchi S, Murakami N, Yamashita H, Toda M, Kawamoto H. Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg. 1998; 133:276–80.5. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Preoperative ultrasonographic examination for lymph node metastasis: usefulness when designing lymph node dissection for papillary microcarcinoma of the thyroid. World J Surg. 2004; 28:498–501.6. Haugen BR, Alexander EK, Bible KC, Doherty G, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2015. [Epub ahead of print].7. Moreno MA, Agarwal G, de Luna R, Siegel ER, Sherman SI, Edeiken-Monroe BS, et al. Preoperative lateral neck ultrasonography as a longterm outcome predictor in papillary thyroid cancer. Arch Otolaryngol Head Neck Surg. 2011; 137:157–62.
Article8. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Ultrasonographically and anatomopathologically detectable node metastases in the lateral compartment as indicators of worse relapse-free survival in patients with papillary thyroid carcinoma. World J Surg. 2005; 29:917–20.
Article9. Lee K, Kawata R, Nishikawa S, Yoshimura K, Takenaka H. Diagnostic criteria of ultrasonographic examination for lateral node metastasis of papillary thyroid carcinoma. Acta Otolaryngol. 2010; 130:161–6.
Article10. Ito Y, Miyauchi A. Lateral and mediastinal lymph node dissection in differentiated thyroid carcinoma: indications, benefits, and risks. World J Surg. 2007; 31:905–15.
Article11. Park JS, Son KR, Na DG, Kim E, Kim S. Performance of preoperative sonographic staging of papillary thyroid carcinoma based on the sixth edition of the AJCC/UICC TNM classification system. AJR Am J Roentgenol. 2009; 192:66–72.
Article12. Stulak JM, Grant CS, Farley DR, Thompson GB, van Heerden JA, Hay ID, et al. Value of preoperative ultrasonography in the surgical management of initial and reoperative papillary thyroid cancer. Arch Surg. 2006; 141:489–94.
Article13. Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A. A novel classification system for patients with PTC: addition of the new variables of large (3 cm or greater) nodal metastases and reclassification during the follow-up period. Surgery. 2004; 135:139–48.
Article14. Hunt JP, Buchmann LO, Wang L, Abraham D. An analysis of factors predicting lateral cervical nodal metastases in papillary carcinoma of the thyroid. Arch Otolaryngol Head Neck Surg. 2011; 137:1141–5.
Article15. Sivanandan R, Soo KC. Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg. 2001; 88:1241–4.
Article16. Kupferman ME, Patterson M, Mandel SJ, LiVolsi V, Weber RS. Patterns of lateral neck metastasis in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 2004; 130:857–60.
Article17. Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg. 1998; 85:252–4.
Article18. Shaha AR. Management of the neck in thyroid cancer. Otolaryngol Clin North Am. 1998; 31:823–31.
Article19. Lim YS, Lee JC, Lee YS, Lee BJ, Wang SG, Son SM, et al. Lateral cervical lymph node metastases from papillary thyroid carcinoma: predictive factors of nodal metastasis. Surgery. 2011; 150:116–21.
Article20. Zeng RC, Zhang W, Gao EL, Cheng P, Huang GL, Zhang XH, et al. Number of central lymph node metastasis for predicting lateral lymph node metastasis in papillary thyroid microcarcinoma. Head Neck. 2014; 36:101–6.
Article21. Xiao GZ, Gao L. Central lymph node metastasis: is it a reliable indicator of lateral node involvement in papillary thyroid carcinoma? World J Surg. 2010; 34:237–41.
Article22. Zafon C, Obiols G, Baena JA, Castellví J, Dalama B, Mesa J. Preoperative thyrotropin serum concentrations gradually increase from benign thyroid nodules to papillary thyroid microcarcinomas then to papillary thyroid cancers of larger size. J Thyroid Res. 2012; 2012:530721.
Article23. Fiore E, Rago T, Provenzale MA, Scutari M, Ugolini C, Basolo F, et al. Lower levels of TSH are associated with a lower risk of papillary thyroid cancer in patients with thyroid nodular disease: thyroid autonomy may play a protective role. Endocr Relat Cancer. 2009; 16:1251–60.
Article24. Boelaert K, Horacek J, Holder RL, Watkinson JC, Sheppard MC, Franklyn JA. Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J Clin Endocrinol Metab. 2006; 91:4295–301.
Article25. Haymart MR, Glinberg SL, Liu J, Sippel RS, Jaume JC, Chen H. Higher serum TSH in thyroid cancer patients occurs independent of age and correlates with extrathyroidal extension. Clin Endocrinol (Oxf). 2009; 71:434–9.
Article26. Haymart MR, Repplinger DJ, Leverson GE, Elson DF, Sippel RS, Jaume JC, et al. Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J Clin Endocrinol Metab. 2008; 93:809–14.
Article27. Kim SS, Lee BJ, Lee JC, Song SH, Kim BH, Son SM, et al. Preoperative serum thyroid stimulating hormone levels in well-differentiated thyroid carcinoma is a predictive factor for lateral lymph node metastasis as well as extrathyroidal extension in Korean patients: a singlecenter experience. Endocrine. 2011; 39:259–65.
Article28. Gerschpacher M, Göbl C, Anderwald C, Gessl A, Krebs M. Thyrotropin serum concentrations in patients with papillary thyroid microcancers. Thyroid. 2010; 20:389–92.
Article29. Lin HY, Tang HY, Shih A, Keating T, Cao G, Davis PJ, et al. Thyroid hormone is a MAPK-dependent growth factor for thyroid cancer cells and is antiapoptotic. Steroids. 2007; 72:180–7.
Article30. Lai V, Yen TW, Rose BT, Fareau GG, Misustin SM, Evans DB, et al. The Effect of Thyroiditis on the Yield of Central Compartment Lymph Nodes in Patients with Papillary Thyroid Cancer. Ann Surg Oncol. 2015; 22:4181–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
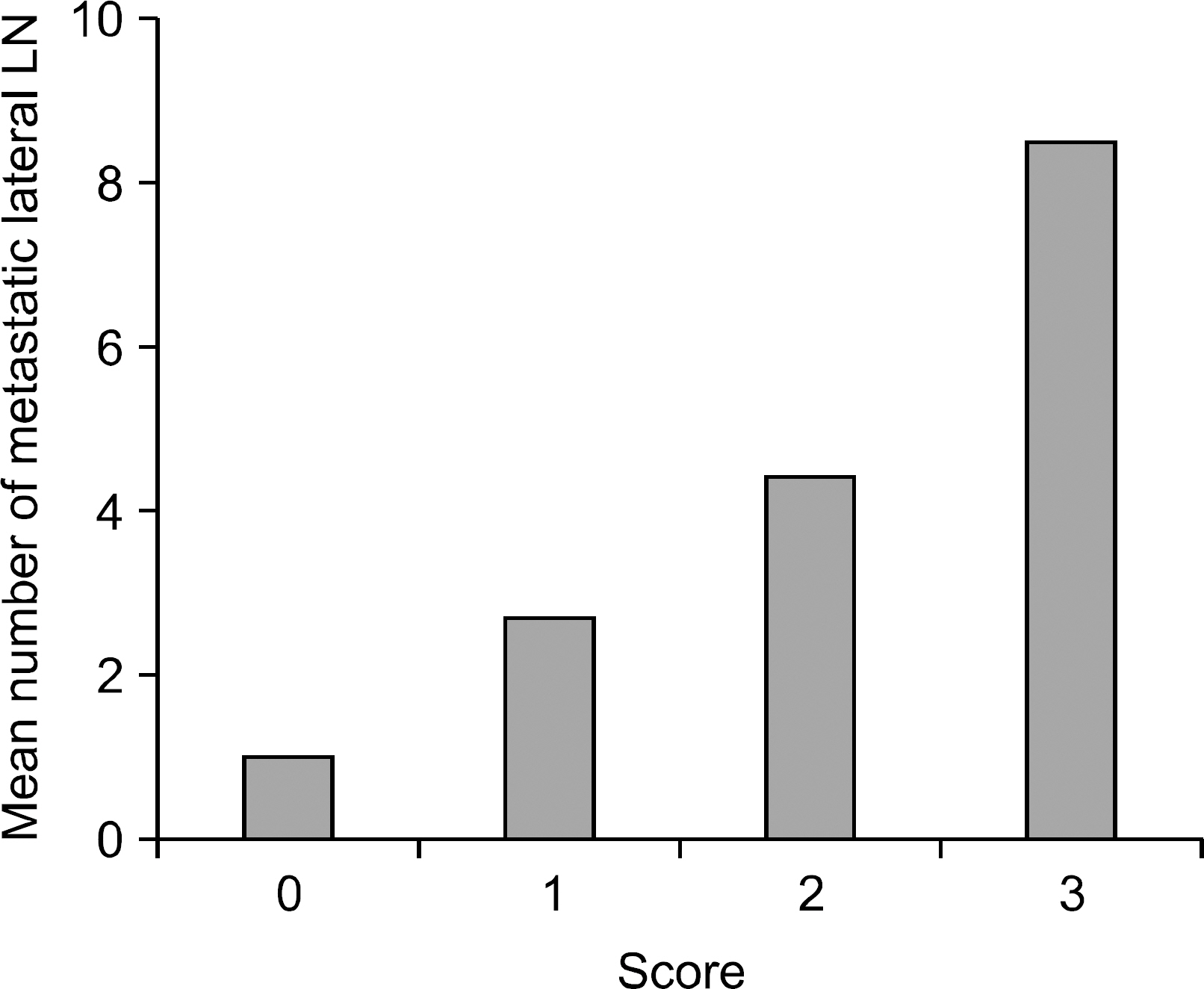
- A Scoring System for Prediction of Lateral Neck Node Metastasis from Papillary Thyroid Cancer
- The Pattern of Cervical Lymph Node Metastases in Papillary Thyroid Cancer
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer
- The Diagnostic Utility of Ultrasonography, CT and PET/CT for the Preoperative Evaluation of Cervical Lymph Node Metastasis in Papillary Thyroid Cancer Patients
- The Clinical Significance of Scored CT Findings for Pre-operative Prediction of Lateral Cervical Lymph Node Metastasis in Thyroid Cancer