J Korean Med Sci.
2013 Jan;28(1):87-92. 10.3346/jkms.2013.28.1.87.
Peripheral Artery Disease in Korean Patients Undergoing Percutaneous Coronary Intervention: Prevalence and Association with Coronary Artery Disease Severity
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. sh1214.choi@samsung.com
- KMID: 2158006
- DOI: http://doi.org/10.3346/jkms.2013.28.1.87
Abstract
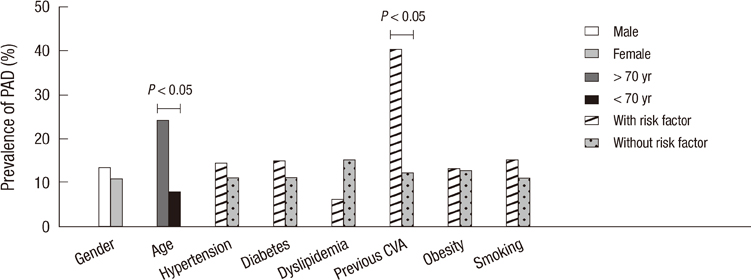
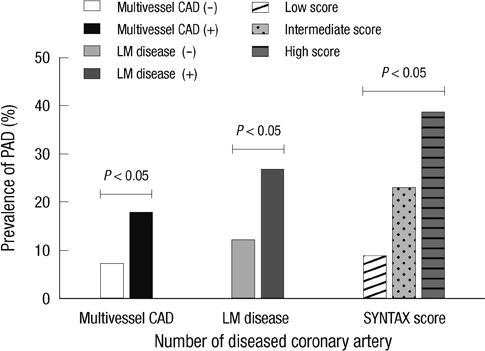
- Peripheral artery disease (PAD) is an important marker for the risk stratification of patients with coronary artery disease (CAD). We investigated the prevalence of PAD in patients undergoing percutaneous coronary intervention (PCI) with CAD and the relationship between ankle-brachial pressure index (ABPI) and CAD severity. A total of 711 patients undergoing PCI for CAD from August 2009 to August 2011 were enrolled. PAD diagnosis was made using the ABPI. The prevalence of PAD was 12.8%. In PAD patients, mean values of right and left ABPI were 0.71 +/- 0.15 and 0.73 +/- 0.15. Patients with PAD had a higher prevalence of left main coronary disease (14.3% vs 5.8%, P = 0.003), more frequently had multivessel lesions (74.9% vs 52.1%, P < 0.001) and had higher SYNTAX score (18.2 +/- 12.3 vs 13.1 +/- 8.26, P = 0.002). Using multivariate analysis, we determined that left main CAD (OR, 2.954; 95% CI, 1.418-6.152, P = 0.004) and multivessel CAD (OR, 2.321; 95% CI, 1.363-3.953, P = 0.002) were both independently associated with PAD. We recommend that ABPI-based PAD screening should be implemented in all patients undergoing PCI with CAD, especially in severe cases.
MeSH Terms
-
Aged
Ankle Brachial Index
Asian Continental Ancestry Group
Coronary Artery Disease/*diagnosis/epidemiology/etiology
Female
Humans
Male
Middle Aged
Multivariate Analysis
Odds Ratio
Percutaneous Coronary Intervention
Peripheral Arterial Disease/complications/*diagnosis/epidemiology
Prevalence
Republic of Korea/epidemiology
Risk Factors
Severity of Illness Index
Figure
Reference
-
1. Kennedy M, Solomon C, Manolio TA, Criqui MH, Newman AB, Polak JF. Risk factors for declining ankle-brachial index in men and women 65 years or older: the cardiovascular health study. Arch Intern Med. 2005. 165:1896–1902.2. Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the strong heart study. Circulation. 2004. 109:733–739.3. Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, Paranandi L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA. 1992. 267:2344–2348.4. Salasidis GC, Latter DA, Steinmetz OK, Blair JF, Graham AM. Carotid artery duplex scanning in preoperative assessment for coronary artery revascularization: the association between peripheral vascular disease, carotid artery stenosis, and stroke. J Vasc Surg. 1995. 21:154–160.5. Eagle KA, Rihal CS, Foster ED, Mickel MC, Gersh BJ. Long-term survival in patients with coronary artery disease: importance of peripheral vascular disease. The coronary artery surgery study (cass) investigators. J Am Coll Cardiol. 1994. 23:1091–1095.6. Jeremias A, Gruberg L, Patel J, Connors G, Brown DL. Effect of peripheral artery disease on in-hospital outcomes after primary percutaneous coronary intervension for acute myocardial infarction. Am J Cardiol. 2010. 105:1268–1271.7. Saw J, Bhatt DL, Moliterno DJ, Brener SJ, Steinhubl SR, Lincoff AM, Tcheng JE, Harrington RA, Simoons M, Hu T, et al. The influence of peripheral artery disease on outcomes: a pooled analysis of mortality in eight large randomized percutaneous coronary intervention trials. J Am Coll Cardiol. 2006. 48:1567–1572.8. McDermott MM, Liu K, Criqui MH, Ruth K, Goff D, Saad MF. Ankle-brachial index and subclinical cardiac and carotid disease: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2005. 162:33–41.9. Hirsch AT, Criqui MH, Treat-Jacobson D, Regensteiner JG, Creager MA, Olin JW. Peripheral artery disease detection, awareness, and treatment in primary care. JAMA. 2001. 286:1317–1324.10. Atmer B, Jogestrand T, Laska J, Lund F. Peripheral artery disease in patients with coronary artery disease. Int Angiol. 1995. 14:89–93.11. Girasis C, Garg S, Räber L, Sarno G, Morel MA, Garcia HM, Lüscher TF, Serruys PW, Windecker S. SYNTAX score and Clinical SYNTAX score as predictors of very long-term clinical outcomes in patients undergoing percutaneous coronary interventions: a substudy of SIRolimus-eluting stent compared with pacliTAXel-eluting stent for coronary revascularization (SIRTAX) trial. Eur Heart J. 2011. 32:3115–3127.12. Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, Van Dyck N, Russell ME, Mohr FW, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005. 1:219–227.13. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009. 5:50–56.14. Ahn S, Park YJ, Min SI, Kim SY, Ha J, Kim SJ, Kim HS, Yoon BW, Min SK. High prevalence of peripheral artery disease in Korean patients with coronary or cerebrovascular disease. J Korean Med Sci. 2012. 27:625–629.15. Dieter RS, Tomasson J, Gudjonsson T, Brown RL, Vitcenda M, Einerson J. Lower extremity peripheral artery disease in hospitalized patients with coronary artery disease. Vasc Med. 2003. 8:233–236.16. Huelmos A, Jimenez J, Guijarro C, Belinchon JC, Puras E, Sanchez C. Underrecognized peripheral artery disease in patients with acute coronary syndrome: Prevalence of traditional and emergent cardiovascular risk factors. Rev Esp Cardiol. 2005. 58:1403–1410.17. Hong YM. Atherosclerotic cardiovascular disease beginning in childhood. Korean Circ J. 2010. 40:1–9.18. Leng GC, Fowkes FG, Lee AJ, Dunbar J, Housley E, Ruckley CV. Use of ankle brachial pressure index to predict cardiovascular events and death: A cohort study. BMJ. 1996. 313:1440–1444.19. Koo SH, Gil TY, Lee HW, Lee K, Hong YM. Effects of smoking on the pulse wave velocity and ankle brachial index in adolescents. Korean Circ J. 2007. 37:414–418.20. Moussa ID, Jaff MR, Mehran R, Gray W, Dangas G, Lazic Z. Prevalence and prediction of previously unrecognized peripheral artery disease in patients with coronary artery disease: the peripheral artery disease in interventional patients study. Catheter Cardiovasc Interv. 2009. 73:719–724.21. Brooks B, Dean R, Patel S, Wu B, Molyneaux L, Yue DK. TBI or not TBI: that is the question. Is it better to measure toe pressure than ankle pressure in diabetic patients? Diabet Med. 2001. 18:528–532.22. Aboyans V, Ho E, Denenberg JO, Ho LA, Natarajan L, Criqui MH. The association between elevated ankle systolic pressures and peripheral occlusive artery disease in diabetic and nondiabetic subjects. J Vasc Surg. 2008. 48:1197–1203.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- Diabetes Mellitus and Coronary Angiography
- Frequency of Combined Atherosclerotic Disease of the Coronary, Periphery, and Carotid Arteries Found by Angiography
- Diffuse Long Coronary Artery Disease is Still an Obstacle for Percutaneous Coronary Intervention in the Second-Generation Drug-Eluting Stent Era?
- Past, Present, and Future of Left Main Coronary Artery PCI