J Korean Med Sci.
2012 Nov;27(11):1428-1432. 10.3346/jkms.2012.27.11.1428.
The Return of an Old Worm: Cerebral Paragonimiasis Presenting with Intracerebral Hemorrhage
- Affiliations
-
- 1Division of Pediatric Neurosurgery, Seoul National University Children's Hospital, Seoul, Korea. phi.jihoon@gmail.com
- 2Department of Parasitology and Tropical Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Diagnostic Radiology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2157958
- DOI: http://doi.org/10.3346/jkms.2012.27.11.1428
Abstract
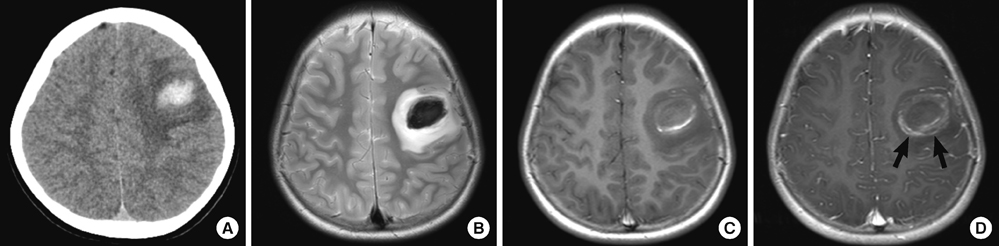
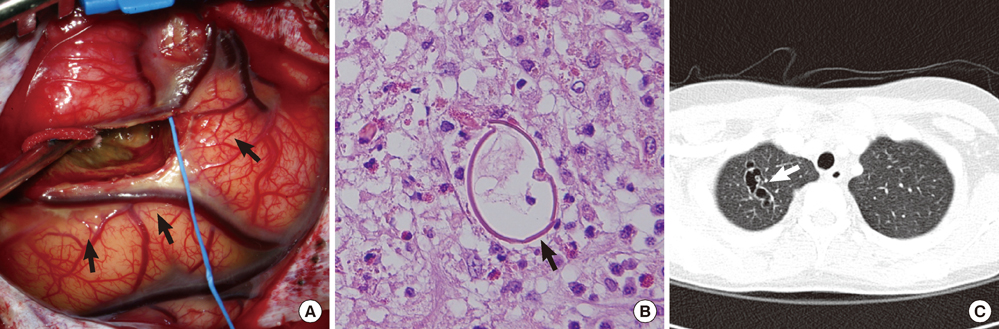
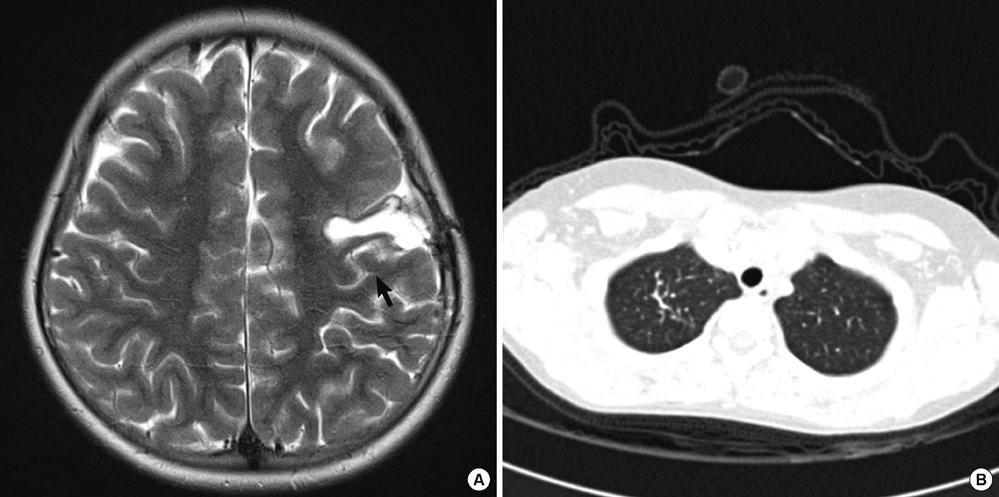
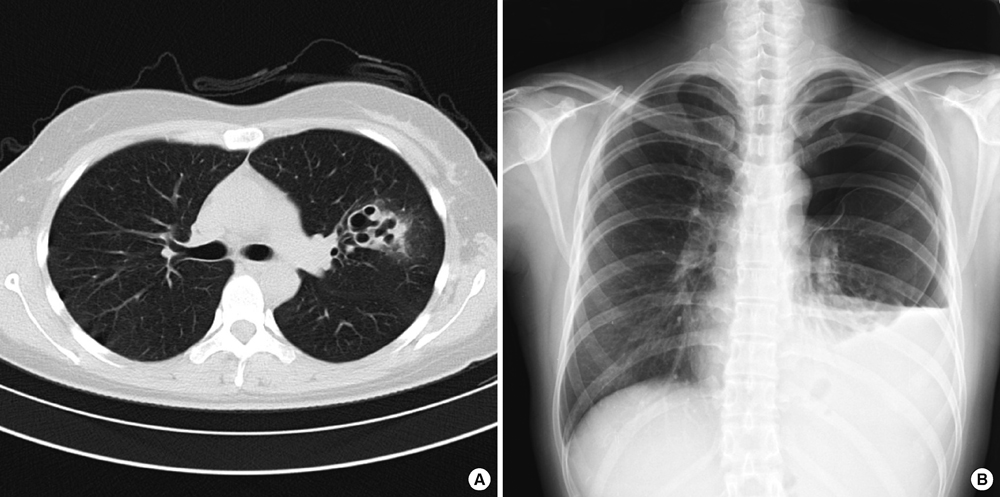
- Paragonimiasis is caused by ingesting crustaceans, which are the intermediate hosts of Paragonimus. The involvement of the brain was a common presentation in Korea decades ago, but it becomes much less frequent in domestic medical practices. We observed a rare case of cerebral paragonimiasis manifesting with intracerebral hemorrhage. A 10-yr-old girl presented with sudden-onset dysarthria, right facial palsy and clumsiness of the right hand. Brain imaging showed acute intracerebral hemorrhage in the left frontal area. An occult vascular malformation or small arteriovenous malformation compressed by the hematoma was initially suspected. The lesion progressed for over 2 months until a delayed surgery was undertaken. Pathologic examination was consistent with cerebral paragonimiasis. After chemotherapy with praziquantel, the patient was monitored without neurological deficits or seizure attacks for 6 months. This case alerts practicing clinicians to the domestic transmission of a forgotten parasitic disease due to environmental changes.
MeSH Terms
-
Animals
Anthelmintics/therapeutic use
Brain/parasitology/pathology
Cerebral Hemorrhage/*etiology
Child
Dysarthria/etiology
Facial Paralysis/etiology
Female
Humans
Magnetic Resonance Imaging
Paragonimiasis/*diagnosis/drug therapy/parasitology
Paragonimus/isolation & purification
Praziquantel/therapeutic use
Tomography, X-Ray Computed
Vascular Malformations/etiology
Anthelmintics
Praziquantel
Figure
Reference
-
1. Choi DW. Paragonimus and paragonimiasis in Korea. Korean J Parasitol. 1990. 28:Suppl. 79–102.2. Cha SH, Chang KH, Cho SY, Han MH, Kong Y, Suh DC, Choi CG, Kang HK, Kim MS. Cerebral paragonimiasis in early active stage: CT and MR features. AJR Am J Roentgenol. 1994. 162:141–145.3. Oh SJ. Cerebral paragonimiasis. J Neurol Sci. 1969. 8:27–48.4. Park J, Miyagawa T, Hong J, Kim O. Cerebral paragonimiasis and Bo Sung Sim's hemispherectomy in Korea in 1950s-1960s. Korean J Med Hist. 2011. 20:119–161.5. Kim EM, Kim JL, Choi SI, Lee SH, Hong ST. Infection status of freshwater crabs and crayfish with metacercariae of Paragonimus westermani in Korea. Korean J Parasitol. 2009. 47:425–426.6. Kang SY, Kim TK, Kim TY, Ha YI, Choi SW, Hong SJ. A case of chronic cerebral paragonimiasis westermani. Korean J Parasitol. 2000. 38:167–171.7. Sim BS, Chu CW, Suh YW, Youn KC. Cerebral hemispherectomy for control of intractable convulsions caused by diffuse cerebral paragonimiasis. J Korean Surg Soc. 1962. 4:379–388.8. Lee MK, Hong SJ, Kim HR. Seroprevalence of tissue invading parasitic infections diagnosed by ELISA in Korea. J Korean Med Sci. 2010. 25:1272–1276.9. Lee WJ, Koh EJ, Choi HY. Epilepsy surgery of the cerebral paragonimiasis. J Korean Neurosurg Soc. 2006. 39:114–119.10. Lim SH, Cho HC, Lee KY, Lee YJ, Koh SH. Cerebral paragonimiasis presenting as recurrent hemorrhagic stroke without pulmonary symptoms. J Korean Neurol Assoc. 2011. 29:371–373.11. Choo JD, Suh BS, Lee HS, Lee JS, Song CJ, Shin DW, Lee YH. Chronic cerebral paragonimiasis combined with aneurysmal subarachnoid hemorrhage. Am J Trop Med Hyg. 2003. 69:466–469.12. The Hankyoreh. No Paragonimus in well fertilized crabs. 2004. 07. 01. accessed on 8 April 2012. Available at http://legacy.www.hani.co.kr/section-005100033/2004/07/005100033200407011953640.html.13. The Kukminilbo. Be careful for paragonimiasis by eating soybean sauceed crabs: Recent resurge of paragonimiasis patients. 2006. 06. 28. accessed on 19 June 2012. Available at http://news.naver.com/main/read.nhn?mode=LSD&mid=sec&sid1=103&oid=005&aid=0000249546.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microscopic Polyangiitis Presenting with Intracerebral Hemorrhage and Cerebral Infarction
- A Case of Wegener's Granulomatosis Presenting with Cerebral Infarction and Intracerebral Hemorrhage
- Etiology and Pathogenesis of Hypertensive Intracerebral Hemorrhage
- Progressive Manifestations of Reversible Cerebral Vasoconstriction Syndrome Presenting with Subarachnoid Hemorrhage, Intracerebral Hemorrhage, and Cerebral Infarction
- An Experimental Study on Cerebral Paragonimiasis using Cats