J Korean Med Sci.
2006 Aug;21(4):709-714. 10.3346/jkms.2006.21.4.709.
Clinical and Radiological Manifestations of Osteogenesis Imperfecta Type V
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. tjcho@snu.ac.kr
- 2Department of Pathology, Kyunghee University College of Medicine, Seoul, Korea.
- KMID: 2157825
- DOI: http://doi.org/10.3346/jkms.2006.21.4.709
Abstract
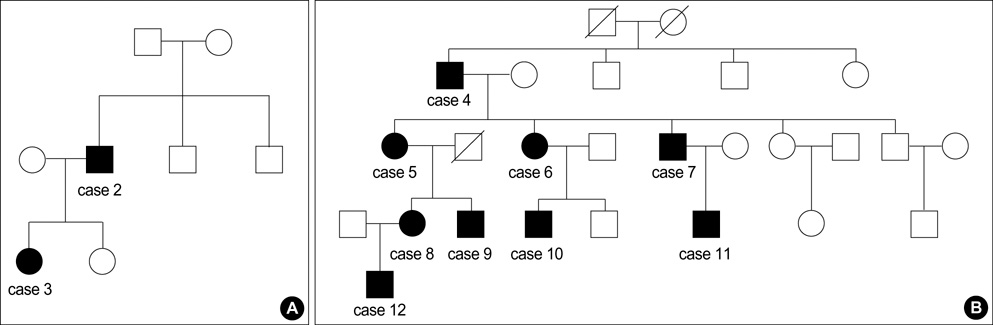
- We reviewed clinical manifestation of 12 patients from three Korean families. They showed mild to moderate bone fragility, and suggested an autosomal dominant inheritance pattern. Significant intrafamilial phenotype variability was obvious. Clinical, radiological, and histopathologic characteristics that distinguished this subtype from others include ossification of interosseous membrane of the forearm with radial head dislocation, hyperplastic callus formation, no evidence of type I collagenopathy and an abnormal histopathologic pattern. Severity of the interosseous membrane ossification was correlated with increasing age (p<0.01) and the radial head dislocation was thought to be a developmental problem rather than a congenital problem. Four children who had bisphosphonate treatment showed improved bone mineral density, radiological changes, and biochemical responses. Osteogenesis imperfecta type V was a distinctive subtype of osteogenesis imperfecta, which caused mild to moderate disability clinically.
Keyword
MeSH Terms
Figure
Reference
-
1. Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979. 16:101–116.
Article2. Shapiro F. Osteogenesis imperfecta in pediatric orthopedic deformities. 2001. Boston: Academic Press;847–860.3. Glorieux FH, Rauch F, Plotokin H, Ward L, Travers R, Roughley P, Lalic L, Glorieux DF, Fassier F, Bishop NJ. Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res. 2000. 15:1650–1658.
Article4. Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley P, Travers R. Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res. 2002. 17:30–38.
Article5. Ward LM, Rauch F, Travers R, Chabot G, Azouz EM, Lalic L, Roughley PJ, Glorieux FH. Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone. 2002. 31:12–18.
Article6. Rauch F, Glorieux FH. Osteogenesis imperfecta. Lancet. 2004. 363:1377–1387.
Article7. References for Korean children's physical development. 1998. Updated Oct. 9, 1998. Retrieved 24 January 2006. Seoul, Korea: Korean Pediatric Society;http://www.pediatrics.or.kr/default.asp .8. National Anthropometric Survey of Korea. 1997. Retrieved January 24, 2006. Seoul, Korea: Korean Agency for Technology and Standards;http://www.standard.go.kr .9. Cho TJ, Choi IH, Chung CY, Yoo WJ, Park MS, Park YK. Efficacy of oral alendronate in children with osteogenesis imperfecta. J Pediatr Orthop. 2005. 25:607–612.
Article10. Cho TJ, Park MS, Choi IH, Chung CY, Yoo WJ. Efficacy of cyclic intravenous pamidronate therapy for children with osteogenesis imperfecta. J Korean Orhtop Assoc. 2003. 38:741–747.
Article11. Fassier AM, Rauch F, Aarabi M, Janelle C, Fassier F. Radial head dislocation in osteogenesis imperfecta. Proceedings of the 9th International Conference on Osteogenesis Imperfecta. 2005. 95.12. Campbell CC, Waters PM, Emans JB. Excision of the radial head for congenital dislocation. J Bone Joint Surg Am. 1992. 74:726–733.
Article13. Glorieux FH, Bishop NJ, Plotkin H, Chabot G, Lanoue G, Travers R. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med. 1998. 339:947–952.
Article14. Zeitlin L, Rauch F, Travers R, Munns C, Glorieux FH. The effect of cyclical intravenous pamidronate in children and adolescents with osteogenesis imperfecta Type V. Bone. 2006. 38:13–20.
Article15. Fleming F, Woodhead HJ, Briody JN, Hall J, Cowell CT, Ault J, Kozlowski K, Sillence DO. Cyclic bisphosphonate therapy in osteogenesis imperfecta type V. J Paediatr Child Health. 2005. 41:147–151.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Osteogenesis Imperfecta: Diagnosed in Uterus by Ultrasonogram
- Intramedullary Nailing in Osteogenesis Imperfecta
- Ostogenesis Imperfecta: Report of 5 Cases
- A Case of Osteogenesis Imperfecta Type II
- Osteogenesis imperfecta and combined orthodontics and orthognathic surgery: a case report on two siblings