J Korean Med Sci.
2004 Aug;19(4):554-559. 10.3346/jkms.2004.19.4.554.
Comparison of Characteristics of Acquired Bilateral Nevus of Ota-like Macules and Nevus of Ota According to Therapeutic Outcome
- Affiliations
-
- 1Department of Dermatology, Ajou University School of Medicine, Suwon, Korea. esl@ajou.ac.kr
- 2Q Skin Clinic, Suwon, Korea.
- KMID: 2157685
- DOI: http://doi.org/10.3346/jkms.2004.19.4.554
Abstract
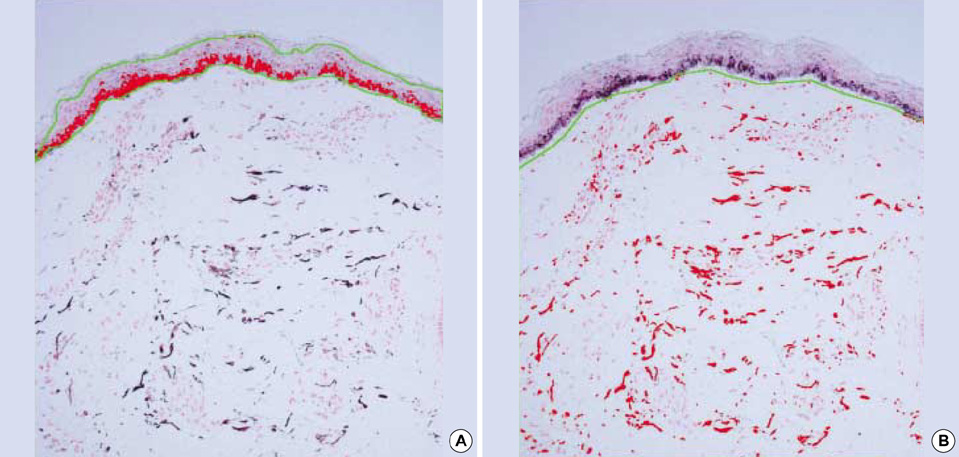
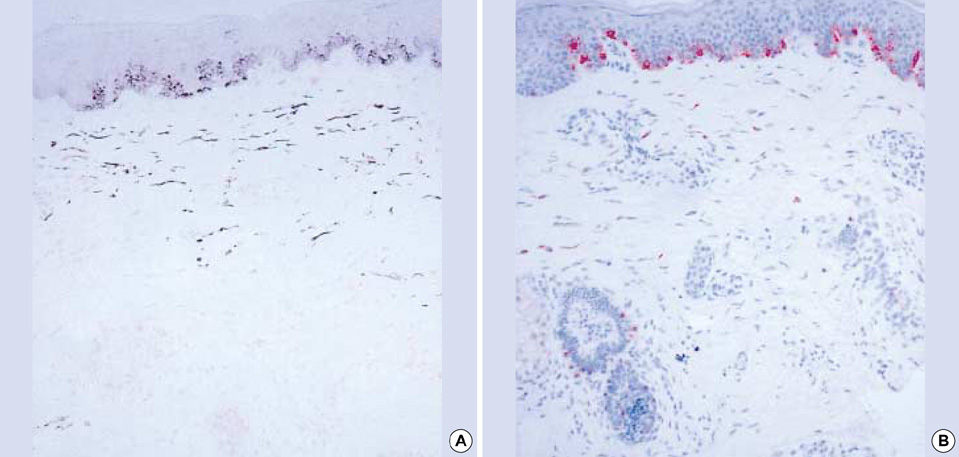
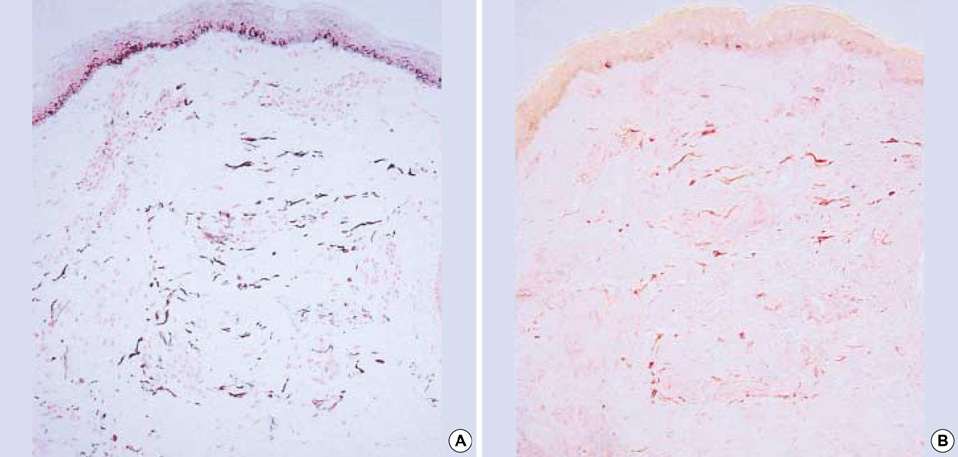
- Both acquired bilateral nevus of Ota-like macules (ABNOM) and nevus of Ota are characterized by the presence of dermal melanocytes. There are no differences in the method of treatment, however, postinflammatory hyperpigmentation (PIH) develops more often in ABNOM than in nevus of Ota following treatment. We investigated the differences in the development of PIH after treatment between ABNOM and nevus of Ota, and the histopathologic differences in the PIH. A total of 82 patients with ABNOM (n=47) and nevus of Ota (n=35) were treated with Q-switched alexandrite laser and followed up 2 weeks and 3 months later. Biopsies were performed on lesional skin before treatment. The distribution and the amount of melanin pigments were visualized with Fontana-Masson stain, and the distribution and the depth of melanocytes were measured by GP-100 (NK1-beteb) stain. Clinically, there was more erythema and PIH in ABNOM than in nevus of Ota. Histopathologically, intradermal melanocytes were clustered in groups and dispersed perivascularly in ABNOM, while melanocytes were scattered evenly throughout the dermis in nevus of Ota. Both groups show that when there is a statistically significant number of melanocytes in the perivascular area, erythema and PIH occur after laser therapy. In conclusion, indirect vessel injury in addition to perivascular clustering melanocytes might be considered the cause of increased PIH after treatment in ABNOM.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Q-Switched Nd:YAG Laser Therapy of Acquired Bilateral Nevus of Ota-like Macules
Woo Jin Lee, Seung Seog Han, Sung Eun Chang, Mi Woo Lee, Jee Ho Choi, Kee Chan Moon, Jai Kyoung Koh
Ann Dermatol. 2009;21(3):255-260. doi: 10.5021/ad.2009.21.3.255.
Reference
-
1. Hori Y, Kawashima M, Oohara K, Kukita A. Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol. 1984. 10:961–964.
Article2. Kunachak S, Kunachakr S, Sirikulchayanonta V, Leelaudomlipi P. Dermabrasion is an effective treatment for acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1996. 22:559–562.
Article3. Anderson RR, Parrish JA. Selective photothermolysis precise microsurgery by selective absorption of pulsed radiation. Science. 1983. 220:524–527.
Article4. Geronemus RG. Q-switched ruby laser therapy of nevus of Ota. Arch Dermatol. 1992. 128:1618–1622.
Article5. Chan HH, King WW, Chan ES, Mok CO, Ho WS, Van Krevel C, Lau WY. In vivo trial comparing patients' tolerance of Q-switched Alexandrite and Q-switched Neodymium: Yttrium-aluminum-Garnet lasers in the treatment of nevus of Ota. Lasers Surg Med. 1999. 24:24–28.6. Chan HH, Ying SY, Ho WS, Kono T, King WW. An in vivo trial comparing the clinical efficacy and complications of Q-switched 755 nm alexandrite and Q-switched 1064 nm Nd:YAG lasers in the treatment of nevus of Ota. Dermatol Surg. 2000. 26:919–922.
Article7. Kunachak S, Leelaudomlipi P, Sirikulchayanonta V. Q-switched ruby laser therapy of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1999. 25:938–941.
Article8. Kunachak S, Leelaudomlipi P. Q-switched Nd:YAG laser treatment for acquired bilateral nevus of Ota-like maculae: a long-term follow-up. Lasers Surg Med. 2000. 26:376–379.
Article9. Polnikorn N, Tanrattanakorn S, Goldberg DJ. Treatment of Hori's nevus with the Q-switched Nd:YAG laser. Dermatol Surg. 2000. 26:477–480.
Article10. Kang W, Lee E, Choi GS. Treatment of Ota's nevus by Q-switched alexandrite laser: therapeutic outcome in relation to clinical and histopathological findings. Eur J Dermatol. 1999. 9:639–643.11. Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched ruby laser. N Engl J Med. 1994. 331:1745–1750.
Article12. Kono T, Nozaki M, Chan HH, Mikashima Y. A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Lasers Surg Med. 2001. 29:156–159.
Article13. Suh DH, Hwang JH, Lee HS, Youn JI, Kim PM. Clinical features of Ota's naevus in Koreans and its treatment with Q-switched alexandrite laser. Clin Exp Dermatol. 2000. 25:269–273.
Article14. Lam AY, Wong DS, Lam LK, Ho WS, Chan HH. A retrospective study on the efficacy and complications of Q-switched alexandrite laser in the treatment of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 2001. 27:937–941.
Article15. Ruiz-Maldonado R, Orozco-Covarrubias ML. Postinflammatory hypopigmentation and hyperpigmentation. Semin Cutan Med Surg. 1997. 16:36–43.
Article16. Kim SD, Kim SW, Huh CH, Suh DH, Eun HC. Changes of biophysical properties of the skin measured by non-invasive techniques after Q-switched Nd-YAG laser therapy in patients with nevus of Ota. Skin Res Technol. 2001. 7:262–271.
Article17. Takiwaki H, Shirai S, Kohno H, Soh H, Arase S. The degrees of UVB-induced erythema and pigmentation correlate linearly and are reduced in a parallel manner by topical anti-inflammatory agents. J Invest Dermatol. 1994. 103:642–646.
Article18. Lu Z, Chen J, Wang X, Fang L, Jiao S, Huang W. Effect of Q-switched alexandrite laser irradiation on dermal melanocytes of nevus of Ota. Chin Med J (Engl). 2000. 113:49–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acquired Bilateral Nevus of Ota-like Macules Accompanying the Common Blue Nevus
- Tree Cases of Aquired bilateral Nevus of Ota-like Marcules
- Acquired, Bilateral Nevus of Ota-like Macules (ABNOM) Associated with Ota's Nevus: Case Report
- A Case of Bilateral Nevus of Ota Associated with Bilateral Nevus of Ito
- A Case of Acquired Bilateral Nevus of Ota-like Macules