Ann Dermatol.
2008 Dec;20(4):167-171. 10.5021/ad.2008.20.4.167.
Clinical Study of Porokeratosis Associated with Immunosuppressive Therapy in Renal Transplant Recipients
- Affiliations
-
- 1Department of Dermatology, Kangnam St. Mary's Hospital, College of Medicine,The Catholic University of Korea, Seoul, Korea. yymmpark@hotmail.com
- 2CNP Skin Clinic, Seoul, Korea.
- KMID: 2156387
- DOI: http://doi.org/10.5021/ad.2008.20.4.167
Abstract
-
BACKGROUND: The etiology of porokeratosis (PK) remains unknown, but immunosuppression is known to be a factor in the pathogenesis of PK and it may also exacerbate PK.
OBJECTIVE
The aim of this study was to examine the clinical characteristics of PK associated with immunosuppressive therapy in renal transplant recipients.
METHODS
A total of 9 renal transplant patients diagnosed with biopsy-proven PK from January 2001 to December 2006 were enrolled. The authors analyzed the patient and medication histories, clinical characteristics, and associated diseases.
RESULTS
The ages of the 9 patients ranged from 38 to 67 years (mean 52 years). All received multi-drug regimens comprised of two or three immunosuppressive agents (steroids, cyclosporine, mycophenolate mofetil, azathioprine and/or tacrolimus). Times between transplantation and the onset of PK ranged from 2 to 9 years (mean 4.1 years). No family history of PK or a history of intense sun-exposure was elicited. The number of the lesions was less than ten in 8 of the 9. Lesions were mainly located in the extremities, though some affected the trunk or neck (3). Three patients had disseminated superficial actinic PK (DSAP), PK Mibelli, or both types. Associated diseases included verruca (4), recurrent herpes simplex (1), actinic keratosis (1), and cutaneous B cell lymphoma (1).
CONCLUSION
The three clinical patterns of PK occurred equally in our patients, namely, coexistent PK Mibelli and DSAP, or the DSAP and Mibelli types as independent forms. Our findings support the notion that the different variants of PK be viewed as parts of a heterogeneous clinical spectrum. Further studies are needed in order to establish the clinical patterns of PK in immunosuppressed patients.
MeSH Terms
-
Actins
Azathioprine
Cyclosporine
Extremities
Herpes Simplex
Humans
Immunosuppression
Immunosuppressive Agents
Keratosis, Actinic
Kidney Transplantation
Lymphoma, B-Cell
Methylmethacrylates
Mycophenolic Acid
Neck
Polystyrenes
Porokeratosis
Transplants
Warts
Actins
Azathioprine
Cyclosporine
Immunosuppressive Agents
Methylmethacrylates
Mycophenolic Acid
Polystyrenes
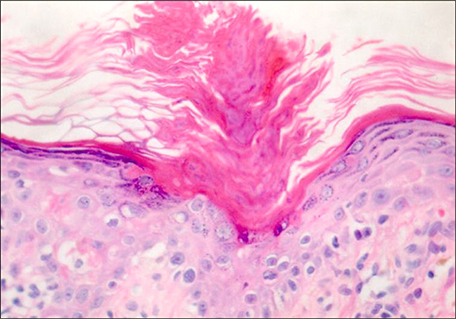
Figure
Reference
-
1. Wolff-Schreiner EC. Porokeratosis. In : Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's dermatology in general medicine. 6th ed. New York: McGraw-Hil;2003. p. 532–537.2. Kanitakis J, Euvrard S, Faure M, Claudy A. Porokeratosis and immunosuppression. Eur J Dermatol. 1998; 8:459–465.3. Manganoni AM, Facchetti F, Gavazzoni R. Involvement of epidermal Langerhans cells in porokeratosis of immunosuppressed renal transplant recipients. J Am Acad Dermatol. 1989; 21:799–801.
Article4. Raychaudhur SP, Smoller BR. Porokeratosis in immunosuppressed and nonimmunosuppressed patients. Int J Dermatol. 1992; 31:781–782.
Article5. Lugo-Janer G, Sanchez JL, Santiago-Delpin E. Prevalence and clinical spectrum of skin diseases in kidney transplant recipients. J Am Acad Dermatol. 1991; 24:410–414.
Article6. Kanitakis J, Euvrard S, Claudy A. Porokeratosis in organ transplant recipients. J Am Acad Dermatol. 2001; 44:144–146.
Article7. Cohen EB, Komorowski RA, Clowry LJ. Cutaneous complications in renal transplant recipients. Am J Clin Pathol. 1987; 88:32–37.
Article8. Herranz P, Pizarro A, De Lucas R, Robayna MG, Rubio FA, Sanz A, et al. High incidence of porokeratosis in renal transplant recipients. Br J Dermatol. 1997; 136:176–179.
Article9. Lee HW, Kim KJ, Lee MW, Choi JH, Moon KC, Koh JK. A case of porokeratosis following heart transplantation. Korean J Dermatol. 2004; 42:1192–1194.10. Song JY, Kim CW, Kim HO. A case of porokeratosis developing after immunosuppression therapy in renal transplant patient. Korean J Dermatol. 2002; 40:224–226.11. Cho YH, Hann SK, Park YK. A case of disseminated superficial porokeratosis in immunosuppressed kidney transplant recipient. Korean J Dermatol. 1992; 30:539–542.12. Sontheimer RD, Bergstresser PR, Gailiunas P Jr, Helderman JH, Gilliam JN. Perturbation of epidermal Langerhans cells in immunosuppressed human renal allograft recipients. Transplantation. 1984; 37:168–174.
Article13. Imakado S, Otsuka F, Ishibashi Y, Ohara K. Abnormal DNA ploidy in cells of the epidermis in a case of porokeratosis. Arch Dermatol. 1988; 124:331–332.
Article14. Kanatakis J. Porokeratosis. In : Euvrard S, Kanitaki J, Claudy A, editors. Skin disease after organ transplantation. Montrouge: John Libbery Eurotext;1998. p. 183–194.15. Sasson M, Krain AD. Porokeratosis and cutaneous malignancy. Dermatol Surg. 1996; 22:339–342.
Article16. Anzai S, Takeo N, Yamaguchi T, Sato T, Takasaki S, Terashi H, et al. Squamous cell carcinoma in a renal transplant recipient with linear porokeratosis. J Dermatol. 1999; 26:244–247.
Article17. Otsuka F, Someya T, Ishibashi Y. Porokeratosis and malignant skin tumors. J Cancer Res Clin Oncol. 1991; 117:55–60.
Article18. Penn I. Skin disorders in organ transplant recipients. External anogenital lesions. Arch Dermatol. 1997; 133:221–223.
Article19. Ferrandiz C, Fuente MJ, Ribera M, Bielsa I, Fernandez MT, Lauzurica R, et al. Epidermal dysplasia and neoplasia in kidney transplant recipients. J Am Acad Dermatol. 1995; 33:590–596.
Article20. Silver SG, Crawford RI. Fatal squamous cell carcinoma arising from transplant-associated porokeratosis. J Am Acad Dermatol. 2003; 49:931–933.
Article21. Nayeemuddin FA, Wong M, Yell J, Rhodes LE. Topical photodynamic therapy in disseminated superficial actinic porokeratosis. Clin Exp Dermatol. 2002; 27:703–706.
Article22. Agrawal SK, Gandhi V, Madan V, Bhattacharya SN. Topical tretinoin in Indian male with zosteriform porokeratosis. Int J Dermatol. 2003; 42:919–920.
Article23. Harrison S, Sinclair R. Porokeratosis of Mibelli: successful treatment with topical 5% imiquimod cream. Australas J Dermatol. 2003; 44:281–283.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cutaneous Manifestations of Kidney Transplant Recipients
- A Case of Porokeratosis Developing after Immunosuppression Therapy in Renal Transplant Patient
- A Case of Exacerbation of Porokeratosis with Myelodysplastic Syndrome
- A case of disseminated superficial porokeratosis in immunosuppressed kidney transplant recipient
- A Concept Analysis of Compliance in Kidney Transplant Recipient Including Compliance with Immunosuppressive Medication