Korean J Crit Care Med.
2015 Nov;30(4):318-322. 10.4266/kjccm.2015.30.4.318.
Spontaneous Lumbar Artery Bleeding and Retroperitoneal Hematoma in a Patient Treated with Continuous Renal Replacement Therapy
- Affiliations
-
- 1Department of Internal Medicine, Daegu Fatima Hospital, Daegu, Korea. dhlee@fatima.or.kr
- 2Department of Radiology, Daegu Fatima Hospital, Daegu, Korea.
- KMID: 2156188
- DOI: http://doi.org/10.4266/kjccm.2015.30.4.318
Abstract
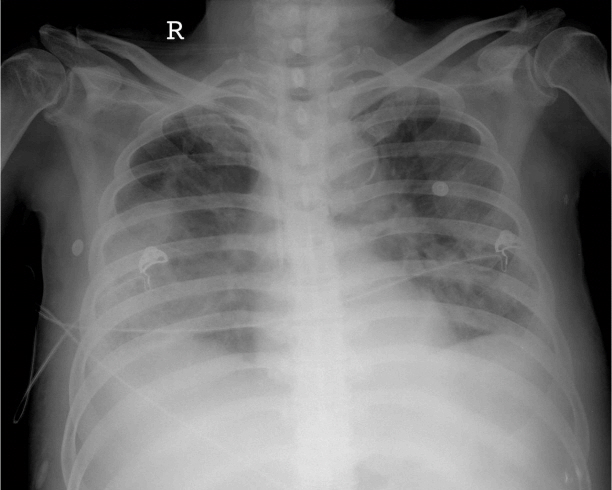
- Rupture of the lumbar artery is usually associated with trauma but rarely has been reported in association with anticoagulation. We present a 71-year-old man who developed spontaneous rupture of the lumbar artery leading to a retroperitoneal hematoma while receiving continuous renal replacement therapy (CRRT). The bleeding was confirmed by computed tomography and angiography and was controlled successfully using selective angiographic embolization. We suggest that spontaneous retroperitoneal bleeding should be considered in a case of sudden decrease in hemoglobin in a CRRT patient.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Sclafani SJ, Florence LO, Phillips TF, Scalea TM, Glanz S, Goldstein AS, et al. Lumbar arterial injury: radiologic diagnosis and management. Radiology. 1987; 165:709–14.
Article2. Fortina M, Carta S, Del Vecchio EO, Crainz E, Urgelli S, Ferrata P. Retroperitoneal hematoma due to spontaneous lumbar artery rupture during fondaparinux treatment. Case report and review of the literature. Acta Biomed. 2007; 78:46–50.3. Pathi R, Voyvodic F, Thompson WR. Spontaneous extraperitoneal haemorrhage: computed tomography diagnosis and treatment by selective arterial embolization. Australas Radiol. 2004; 48:123–8.
Article4. Halak M, Kligman M, Loberman Z, Eyal E, Karmeli R. Spontaneous ruptured lumbar artery in a chronic renal failure patient. Eur J Vasc Endovasc Surg. 2001; 21:569–71.
Article5. Pyo SH, Seo JW, Park JH, Kim KP, Kim SH, Chang JW, et al. Spontaneous rupture of lumbar artery and inferior epigastric artery in a hemodialysis patient. Korean J Nephrol. 2004; 23:992–6.6. Anderson S, Brenner BM. Progressive renal disease: A disorder of adaptation. Q J Med. 1989; 70:185–9.7. Sohal AS, Gangji AS, Crowther MA, Treleaven D. Uremic bleeding: pathophysiology and clinical risk factors. Thromb Res. 2006; 118:417–22.
Article8. Janssen MJ, van der Meulen J. The bleeding risk in chronic haemodialysis: preventive strategies in high-risk patients. Neth J Med. 1996; 48:198–207.
Article9. Bellomo R, Ronco C, Mehta RL. Nomenclature for continuous renal replacement therapies. Am J Kidney Dis. 1996; 28(Suppl 3):S2–7.
Article10. Silverstein ME, Ford CA, Lysaght MJ, Henderson LW. Treatment of severe fluid overload by ultrafiltration. N Engl J Med. 1974; 291:747–51.
Article11. Mehta RL. Anticoagulation strategies for continuous renal replacement therapies: what works? Am J Kidney Dis. 1996; 28(Suppl 3):S8–14.
Article12. Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, et al. Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet. 2000; 356:26–30.
Article13. Bouman CS, Oudemans-Van Straaten HM, Tijssen JG, Zandstra DF, Kesecioglu J. Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med. 2002; 30:2205–11.
Article14. van de Wetering J, Westendorp RG, van der Hoeven JG, Stolk B, Feuth JD, Chang PC. Heparin use in continuous renal replacement procedures: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol. 1996; 7:145–50.
Article15. Davenport A, Will EJ, Davison AM. Comparison of the use of standard heparin and prostacyclin anticoagulation in spontaneous and pump-driven extracorporeal circuits in patients with combined acute renal and hepatic failure. Nephron. 1994; 66:431–7.
Article16. Martin PY, Chevrolet JC, Suter P, Favre H. Anticoagulation in patients treated by continuous venovenous hemofiltration: a retrospective study. Am J Kidney Dis. 1994; 24:806–12.
Article17. Oudemans-van Straaten HM, Wester JP, de Pont AC, Schetz MR. Anticoagulation strategies in continuous renal replacement therapy: can the choice be evidence based? Intensive Care Med. 2006; 32:188–202.
Article18. Reddy BV, Grossman EJ, Trevino SA, Hursting MJ, Murray PT. Argatroban anticoagulation in patients with heparin-induced thrombocytopenia requiring renal replacement therapy. Ann Pharmacother. 2005; 39:1601–5.
Article19. Ohtake Y, Hirasawa H, Sugai T, Oda S, Shiga H, Matsuda K, et al. Nafamostat mesilate as anticoagulant in continuous hemofiltration and continuous hemodiafiltration. Contrib Nephrol. 1991; 93:215–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Rupture of Lumbar Artery & Inferior Epigastric Artery in a Hemodialysis Patient
- Erratum: Spontaneous Lumbar Artery Bleeding and Retroperitoneal Hematoma in a Patient Treated with Continuous Renal Replacement Therapy
- Spontaneous Retroperitoneal Hematoma due to Liver Cirrhosis: A Case Report
- Abdominal Compartment Syndrome Due to Spontaneous Retroperitoneal Hemorrhage in a Patient Undergoing Anticoagulation
- A case of retroperitoneal hematoma by spontaneous rupture of renal capsule in hemorrhagic fever with renal syndrome presented with anuria and unilateral flank pain