Korean J Crit Care Med.
2015 Nov;30(4):303-307. 10.4266/kjccm.2015.30.4.303.
Successful Application of Extracorporeal Membrane Oxygenation for a Patient with Clinical Amniotic Fluid Embolism
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 2Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. cmcksc@gmail.com
- KMID: 2156185
- DOI: http://doi.org/10.4266/kjccm.2015.30.4.303
Abstract
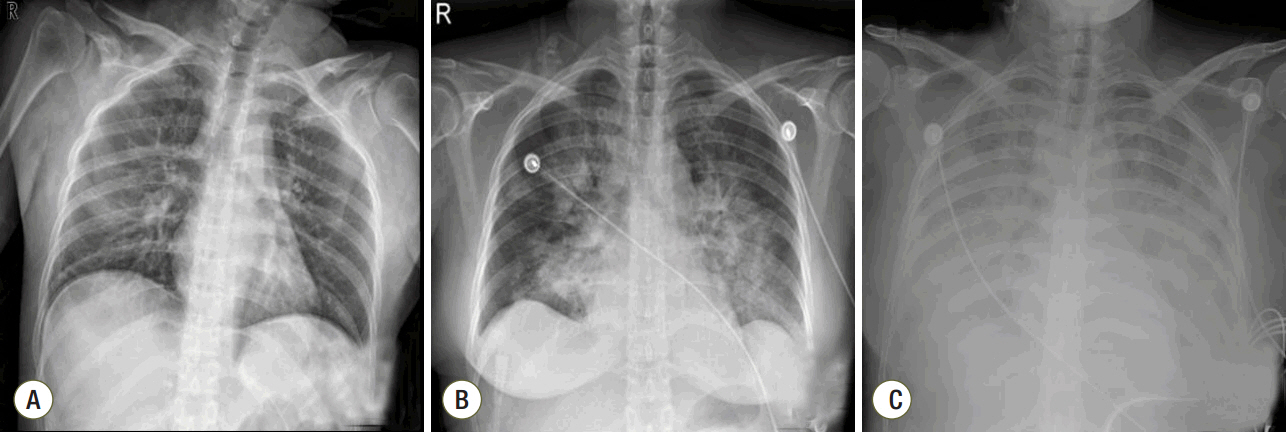
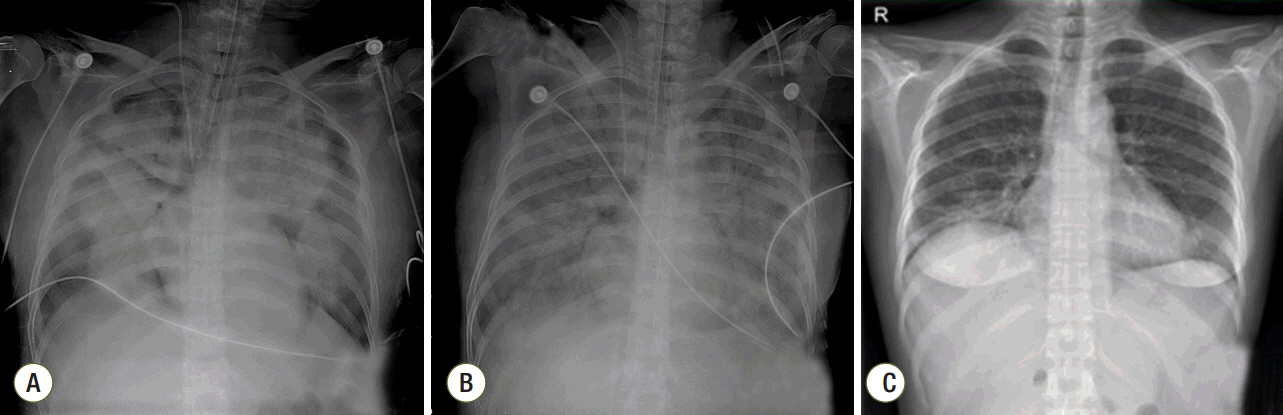
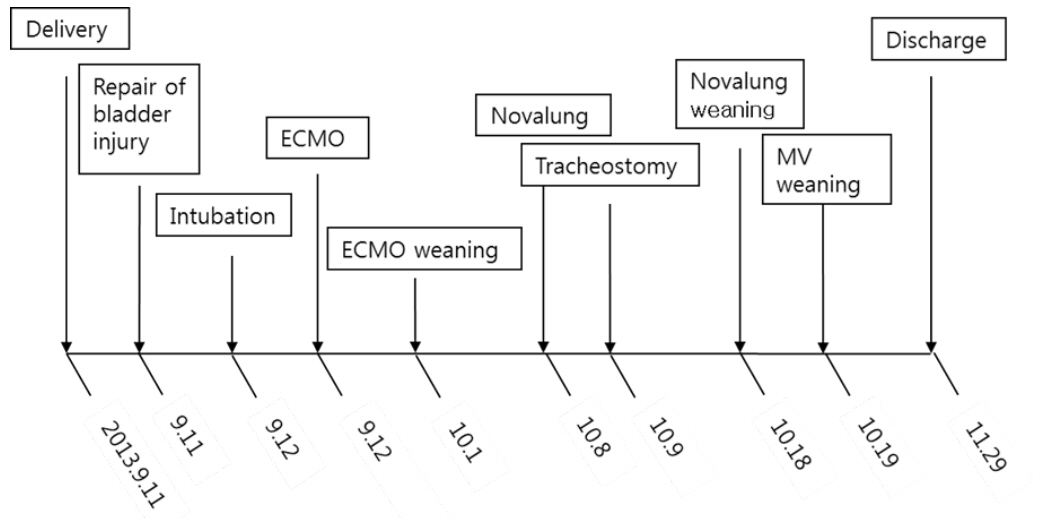
- Amniotic fluid embolism (AFE) is a rare but potentially fatal complication that occurs acutely during pregnancy or within 12 h of delivery. The management of AFE focuses initially on supportive measures for cardiopulmonary stabilization. Extracorporeal membrane oxygenation should be considered in patients who are unresponsive to medical treatment in order to prevent additional hypoxia and subsequent organ failure. We present a 41-year-old woman with clinical AFE who developed acute respiratory distress syndrome and was treated successfully with extracorporeal membrane oxygenation.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Urgent Application of Extracorporeal Membrane Oxygenation in Amniotic Fluid Embolism
Moo Suk Park
Korean J Crit Care Med. 2016;31(3):179-180. doi: 10.4266/kjccm.2016.00745.Venous Air Embolism Not Amniotic Fluid Embolism
Charles Her
Korean J Crit Care Med. 2016;31(1):68-70. doi: 10.4266/kjccm.2016.31.1.68.
Reference
-
References
1. Kanayama N, Tamura N. Amniotic fluid embolism: pathophysiology and new strategies for management. J Obstet Gynaecol Res. 2014; 40:1507–17.
Article2. Moore J, Baldisseri MR. Amniotic fluid embolism. Crit Care Med. 2005; 33(10 Suppl):S279–85.
Article3. Clark SL, Hankins GD, Dudley DA, Dildy GA, Porter TF. Amniotic fluid embolism: analysis of the national registry. Am J Obstet Gynecol. 1995; 172(4 Pt 1):1158–67. discussion 1167-9.
Article4. Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014; 123(2 Pt 1):337–48.
Article5. Conde-Agudelo A, Romero R. Amniotic fluid embolism: an evidence-based review. Am J Obstet Gynecol. 2009; 201:445. e1-13.
Article6. Pantaleo G, Luigi N, Federica T, Paola S, Margherita N, Tahir M. Amniotic fluid embolism: review. Curr Pharm Biotechnol. 2014; 14:1163–7.
Article7. de Swiet M. Maternal mortality: confidential enquiries into maternal deaths in the United Kingdom. Am J Obstet Gynecol. 2000; 182:760–6.
Article8. Yoneyama K, Sekiguchi A, Matsushima T, Kawase R, Nakai A, Asakura H, et al. Clinical characteristics of amniotic fluid embolism: an experience of 29 years. J Obstet Gynaecol Res. 2014; 40:1862–70.9. Ho CH, Chen KB, Liu SK, Liu YF, Cheng HC, Wu RS. Early application of extracorporeal membrane oxygenation in a patient with amniotic fluid embolism. Acta Anaesthesiol Taiwan. 2009; 47:99–102.
Article10. Hsieh YY, Chang CC, Li PC, Tsai HD, Tsai CH. Successful application of extracorporeal membrane oxygenation and intra-aortic balloon counterpulsation as lifesaving therapy for a patient with amniotic fluid embolism. Am J Obstet Gynecol. 2000; 183:496–7.
Article11. Ecker JL, Solt K, Fitzsimons MG, MacGillivray TE. Case records of the Massachusetts General Hospital. Case 40-2012. A 43-year-old woman with cardiorespiratory arrest after a cesarean section. N Engl J Med. 2012; 367:2528–36.12. Reyftmann L, Morau E, Dechaud H, Frapier JM, Hedon B. Extracorporeal membrane oxygenation therapy for circulatory arrest due to postpartum hemorrhage. Obstet Gynecol. 2006; 107(2 Pt 2):511–4.
Article13. Ito F, Akasaka J, Koike N, Uekuri C, Shigemitsu A, Kobayashi H. Incidence, diagnosis and pathophysiology of amniotic fluid embolism. J Obstet Gynaecol. 2014; 34:580–4.
Article14. Uszyński M, Zekanowska E, Uszyński W, Kuczyński J. Tissue factor (TF) and tissue factor pathway inhibitor (TFPI) in amniotic fluid and blood plasma: implications for the mechanism of amniotic fluid embolism. Eur J Obstet Gynecol Reprod Biol. 2001; 95:163–6.
Article15. Allen S, Holena D, McCunn M, Kohl B, Sarani B. A review of the fundamental principles and evidence base in the use of extracorporeal membrane oxygenation (ECMO) in critically ill adult patients. J Intensive Care Med. 2011; 26:13–26.
Article16. Sharma NS, Wille KM, Bellot SC, Diaz-Guzman E. Modern use of extracorporeal life support in pregnancy and postpartum. ASAIO J. 2015; 61:110–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urgent Application of Extracorporeal Membrane Oxygenation in Amniotic Fluid Embolism
- Use of Extracorporeal Membrane Oxygenation in a Fulminant Course of Amniotic Fluid Embolism Syndrome Immediately after Cesarean Delivery
- Massive Endobronchial Hemorrhage After Pulmonary Thromboendarterectomy in Chronic Pulmonary Embolism
- Venous Air Embolism Not Amniotic Fluid Embolism
- Amniotic Fluid Embolism