Korean J Radiol.
2015 Aug;16(4):853-859. 10.3348/kjr.2015.16.4.853.
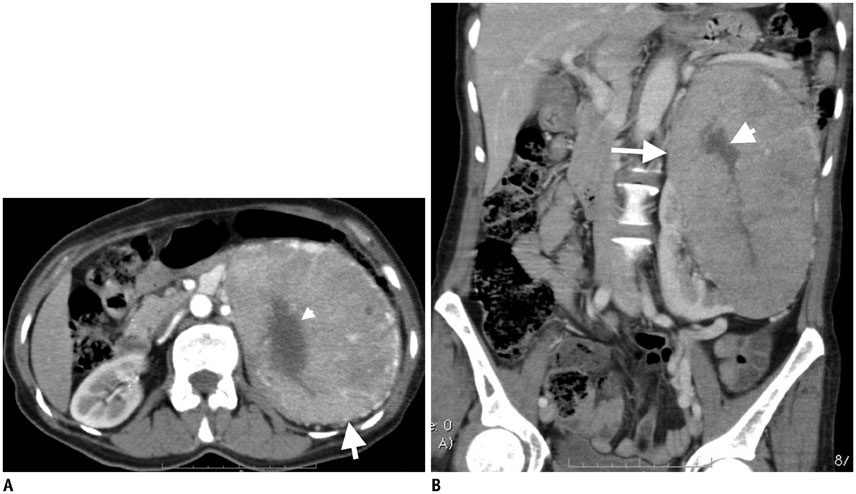
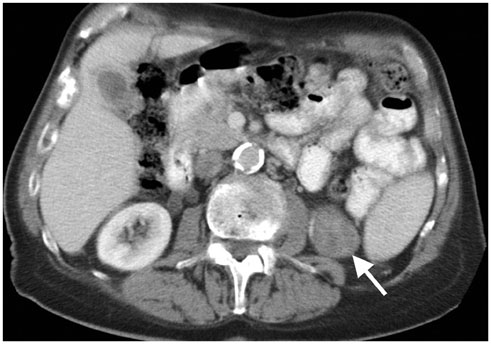
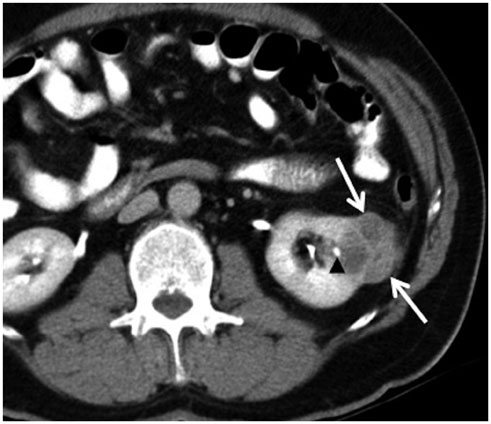
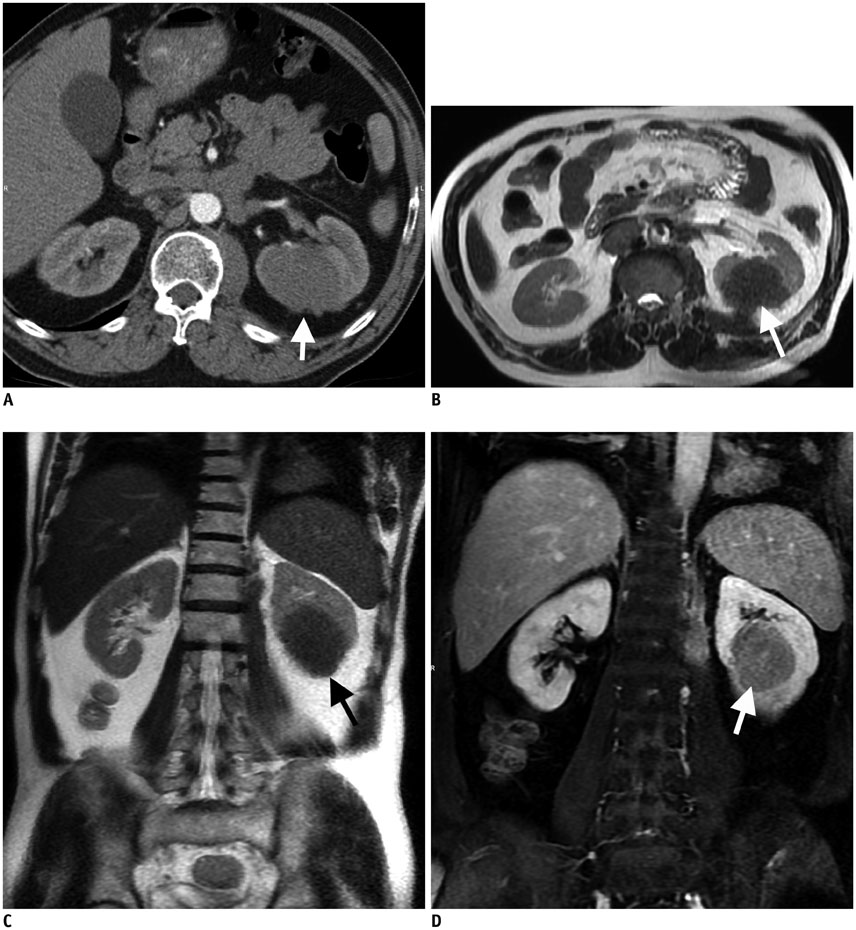
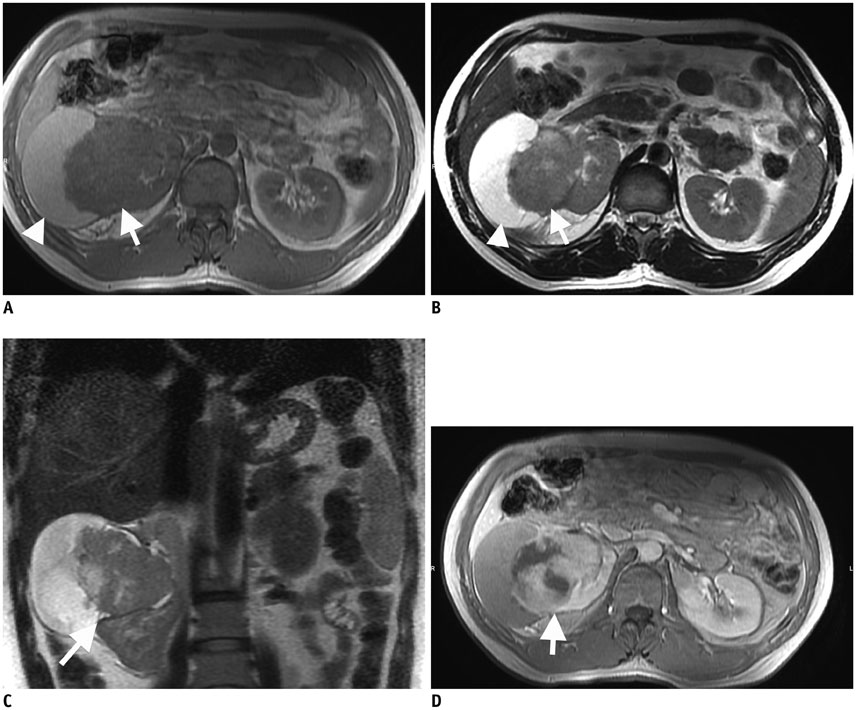
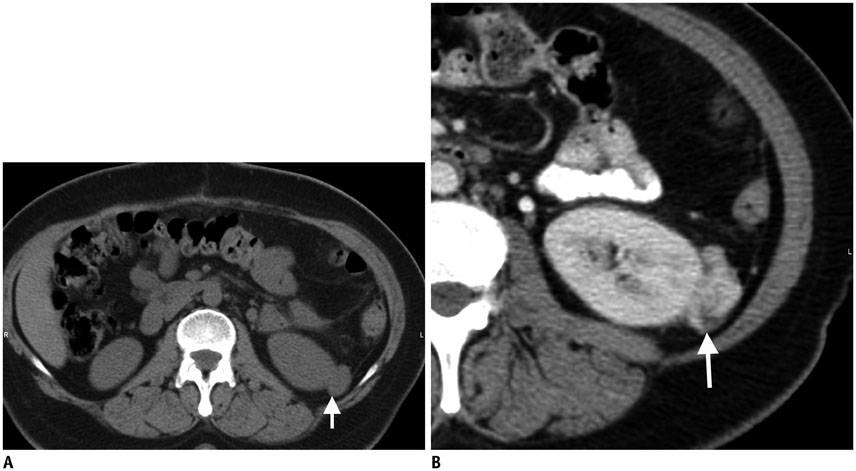
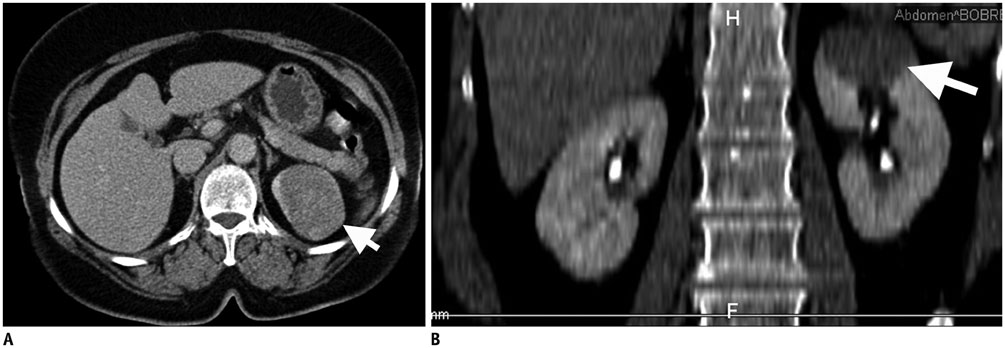
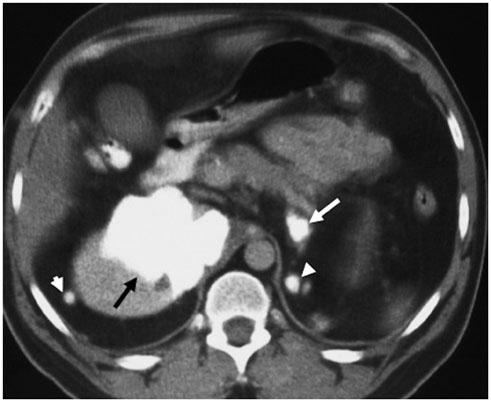
Unusual Malignant Solid Neoplasms of the Kidney: Cross-Sectional Imaging Findings
- Affiliations
-
- 1Department of Radiology, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114, USA.
- 2Department of Radiology, University of Hacettepe School of Medicine, Ankara 06100, Turkey. ruhionur@yahoo.com
- 3Department of Radiology, University of California School of Medicine, Irvine, CA 92697, USA.
- 4Department of Radiology, University of Hacettepe, Faculty of Medicine, Ankara 06100, Turkey.
- KMID: 2155559
- DOI: http://doi.org/10.3348/kjr.2015.16.4.853
Abstract
- Malignant kidney neoplasms are the most frequently encountered solid kidney masses. Although renal cell carcinoma is the major renal malignancy, other solid malignant renal masses should be considered in the differential diagnosis of solid renal masses that do not contain a macroscopic fatty component. In this pictorial essay, we present the imaging findings of a primitive neuroectodermal tumor, primary liposarcoma of the kidney, primary neuroendocrine tumor, leiomyosarcoma, synovial sarcoma, malignant fibrous histiocytoma, sclerosing fibrosarcoma and renal metastasis of osteosarcoma.
MeSH Terms
-
Bone Neoplasms/secondary
Carcinoma, Renal Cell/pathology/radiography
Diagnosis, Differential
Fibrosarcoma/radiography
Histiocytoma/radiography
Humans
Kidney Neoplasms/*pathology/radiography
Leiomyosarcoma/pathology/radiography
Magnetic Resonance Imaging
Middle Aged
Neuroectodermal Tumors, Primitive/pathology/radiography
Osteosarcoma/pathology
Sarcoma
Sarcoma, Synovial/radiography
Tomography, X-Ray Computed
Figure
Reference
-
1. Lee H, Cho JY, Kim SH, Jung DC, Kim JK, Choi HJ. Imaging findings of primitive neuroectodermal tumors of the kidney. J Comput Assist Tomogr. 2009; 33:882–886.2. Pickhardt PJ, Lonergan GJ, Davis CJ Jr, Kashitani N, Wagner BJ. From the archives of the AFIP. Infiltrative renal lesions: radiologic-pathologic correlation. Armed Forces Institute of Pathology. Radiographics. 2000; 20:215–243.3. Chinnaa S, Das CJ, Sharma S, Singh P, Seth A, Purkait S, et al. Peripheral primitive neuroectodermal tumor of the kidney presenting with pulmonary tumor embolism: a case report. World J Radiol. 2014; 6:846–849.4. Dotan ZA, Tal R, Golijanin D, Snyder ME, Antonescu C, Brennan MF, et al. Adult genitourinary sarcoma: the 25-year Memorial Sloan-Kettering experience. J Urol. 2006; 176:2033–2038. discussion 2038-20395. Novick AC, Campbell SC. Renal tumors. In : Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Campbell's urology. 8th ed. Philadelphia: Saunders;2002. p. 2673–2731.6. Ciccarello G, Mucciardi G, Morgia G, Spinelli F, Ascenti G, Macchione L, et al. A case of renal capsular liposarcoma with intracaval fat thrombus. Eur Urol. 2010; 57:350–353.7. Dalal KM, Antonescu CR, Singer S. Diagnosis and management of lipomatous tumors. J Surg Oncol. 2008; 97:298–313.8. Zuetenhorst JM, Taal BG. Metastatic carcinoid tumors: a clinical review. Oncologist. 2005; 10:123–131.9. Osamura RY, Inomoto C, Kajiwara H, DeLellis RA. Neuroendocrine carcinomas of diverse sites. Pathol Case Rev. 2006; 11:282–291.10. Romero FR, Rais-Bahrami S, Permpongkosol S, Fine SW, Kohanim S, Jarrett TW. Primary carcinoid tumors of the kidney. J Urol. 2006; 176(6 Pt 1):2359–2366.11. Kawajiri H, Onoda N, Ohira M, Nakatani T, Wakasa K, Ishikawa T, et al. Carcinoid tumor of the kidney presenting as a large abdominal mass: report of a case. Surg Today. 2004; 34:86–89.12. Kendal WS. The comparative survival of renal leiomyosarcoma. Can J Urol. 2007; 14:3435–3442.13. Katabathina VS, Vikram R, Nagar AM, Tamboli P, Menias CO, Prasad SR. Mesenchymal neoplasms of the kidney in adults: imaging spectrum with radiologic-pathologic correlation. Radiographics. 2010; 30:1525–1540.14. Grasso M, Blanco S, Fortuna F, Crippa S, Di Bella C. Spontaneous rupture of renal leiomyosarcoma in a 45-year-old woman. Arch Esp Urol. 2004; 57:870–872.15. Ochiai K, Onitsuka H, Honda H, Kawamoto K, Uozumi J, Kumazawa J, et al. Leiomyosarcoma of the kidney: CT and MR appearance. J Comput Assist Tomogr. 1993; 17:656–658.16. Lalwani N, Prasad SR, Vikram R, Katabathina V, Shanbhogue A, Restrepo C. Pediatric and adult primary sarcomas of the kidney: a cross-sectional imaging review. Acta Radiol. 2011; 52:448–457.17. Zakhary MM, Elsayes KM, Platt JF, Francis IR. Magnetic resonance imaging features of renal synovial sarcoma: a case report. Cancer Imaging. 2008; 8:45–47.18. Gong J, Kang W, Li S, Yang Z, Xu J. CT findings of synovial sarcomas of the kidney with pathological correlation. Clin Imaging. 2013; 37:1033–1036.19. Murphey MD, Gibson MS, Jennings BT, Crespo-Rodríguez AM, Fanburg-Smith J, Gajewski DA. From the archives of the AFIP: imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics. 2006; 26:1543–1565.20. Froehner M, Manseck A, Haase M, Hakenberg OW, Wirth MP. Locally recurrent malignant fibrous histiocytoma: a rare and aggressive genitourinary malignancy. Urol Int. 1999; 62:164–170.21. Shirkhoda A, Lewis E. Renal sarcoma and sarcomatoid renal cell carcinoma: CT and angiographic features. Radiology. 1987; 162:353–357.22. Eroğlu M, Bakirtaş H, Cimentepe E, Unsal A, Ataoğlu O, Balbay MD. Malignant fibrous histiocytoma arising from the renal capsule. Urol Int. 2005; 75:368–370.23. Kearney MM, Soule EH, Ivins JC. Malignant fibrous histiocytoma: a retrospective study of 167 cases. Cancer. 1980; 45:167–178.24. Kitajima K, Kaji Y, Morita M, Okuda Y, Sugimura K. Malignant fibrous histiocytoma arising from the renal capsule. Magn Reson Med Sci. 2003; 2:199–202.25. Venter A, Roşca E, Muţiu G, Daina L, Pirte A. Difficulties of diagnosis in retroperitoneal tumors. Rom J Morphol Embryol. 2013; 54:451–456.26. Sanyal R, Remer EM. Radiology of the retroperitoneum: case-based review. AJR Am J Roentgenol. 2009; 192:6 Suppl. S112–S117. Quiz S118-S121.27. Chaudhari S, Hatwal D, Suri V. A rare case of primary fibrosarcoma of kidney. Iran J Kidney Dis. 2013; 7:67–69.28. Funston MR, Levine E, Stables DP. Spontaneous renal hemorrhage. Urology. 1976; 8:610–617.29. Raby WN, Kopplin P, Weitzman S. Metastatic osteosarcoma of the kidney presenting as renal hemorrhage. J Pediatr Hematol Oncol. 1996; 18:321–322.30. Jeffree GM, Price CH, Sissons HA. The metastatic patterns of osteosarcoma. Br J Cancer. 1975; 32:87–107.31. Caoili EM, Davenport MS. Role of percutaneous needle biopsy for renal masses. Semin Intervent Radiol. 2014; 31:20–26.32. Lee SW, Lee MH, Yang HJ, Yang WJ, Kim DS, Lee NK, et al. Experience of ultrasonography-guided percutaneous core biopsy for renal masses. Korean J Urol. 2013; 54:660–665.33. Volpe A, Mattar K, Finelli A, Kachura JR, Evans AJ, Geddie WR, et al. Contemporary results of percutaneous biopsy of 100 small renal masses: a single center experience. J Urol. 2008; 180:2333–2337.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidental Solid Renal Masses: Radiologic Assessment and Managements
- Evaluation of malignant intraductal papillary mucinous neoplasms of the pancreas on computed tomography and magnetic resonance imaging
- Unusual tumefactive renal tuberculosis
- Imaging Findings of Pancreatic Solid Pseudopapillary Neoplasm with High-Grade Malignant Transformation: Focusing on Diffusion-Weighted Imaging and Normalized Apparent Diffusion Coefficient Values
- Radiologic-Pathologic Correlation of Unusual Lingual Masses:Part II: Benign and Malignant Tumors