Korean J Urol.
2015 Apr;56(4):310-317. 10.4111/kju.2015.56.4.310.
Elderly men over 65 years of age with late-onset hypogonadism benefit as much from testosterone treatment as do younger men
- Affiliations
-
- 1Global Medical Affairs Andrology, Bayer Pharma AG, Berlin, Germany. farid.saad@bayer.com
- 2Gulf Medical University School of Medicine, Ajman, UAE.
- 3Institute for Urology and Andrology, Norderstedt, Germany.
- 4Dresden International University, Dresden, Germany.
- 5Private Urology Practice, Bremerhaven, Germany.
- 6Department of Epidemiology and Statistics, Boston University School of Public Health, Boston, MA, USA.
- 7Department of Internal Medicine, Endocrine Section, VU medical Center, Amsterdam, The Netherlands.
- KMID: 2155307
- DOI: http://doi.org/10.4111/kju.2015.56.4.310
Abstract
- PURPOSE
To investigate the potential benefits of testosterone administration to elderly men (>65 years) with late-onset hypogonadism (LOH) in comparison with younger men and to assess the safety of testosterone administration to elderly men.
MATERIALS AND METHODS
A total of 561 hypogonadal men from two registry studies were divided into age groups of < or =65 years (group Y, n=450; range, 32-65 years) and >65 years (group O, n=111; range, 66-84 years). Following an initial 6-week interval, all men were treated with 3-month injections of parenteral testosterone undecanoate for up to 6 years.
RESULTS
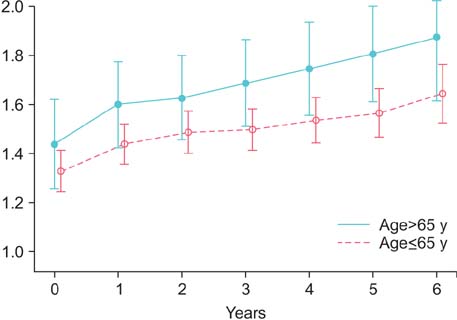
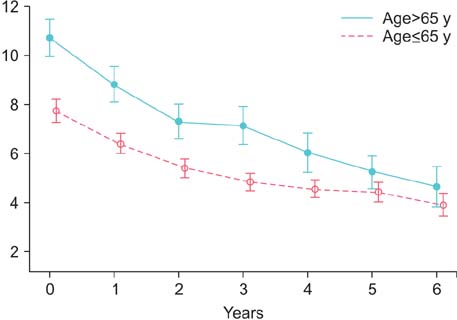
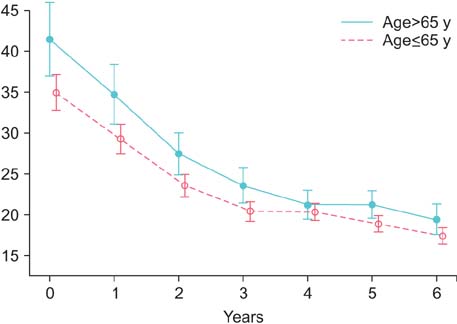
Over the 6 years, there was a progressive decrease of body weight and waist circumference. Beneficial effects on lipids and other metabolic factors and on psychological and sexual functioning progressed over the first 24 to 42 months and were sustained. Rather than a deterioration, there was an improvement of urinary parameters. Prostate volume and prostate-specific antigen increased moderately. Hematocrit levels increased but remained within safe margins.
CONCLUSIONS
The benefits of restoring serum testosterone in men with LOH were not significantly different between men older than 65 years of age and younger men. There were no indications that side effects were more severe in elderly men. The effects on prostate and urinary function and hematocrit were within safe margins. Age itself need not be a contraindication to testosterone treatment of elderly men with LOH.
Keyword
MeSH Terms
-
Age Factors
Age of Onset
Aged
Androgens/administration & dosage
Anthropometry/methods
Drug Monitoring/methods
Germany
Humans
*Hypogonadism/diagnosis/drug therapy/epidemiology/physiopathology/psychology
Male
Middle Aged
Organ Size
*Prostate/drug effects/pathology
Prostate-Specific Antigen/analysis
Registries
*Sexual Behavior/drug effects/psychology
Testosterone/administration & dosage/*analogs & derivatives
Treatment Outcome
Androgens
Testosterone
Prostate-Specific Antigen
Figure
Cited by 1 articles
-
Which Exercise Is Better for Increasing Serum Testosterone Levels in Patients with Erectile Dysfunction?
Jeong Kyun Yeo, Seung Ik Cho, Sun Gu Park, Seok Jo, Jeong Ku Ha, Jeong Woo Lee, Sung Yong Cho, Min Gu Park
World J Mens Health. 2018;36(2):147-152. doi: 10.5534/wjmh.17030.
Reference
-
1. Huhtaniemi I. Late-onset hypogonadism: current concepts and controversies of pathogenesis, diagnosis and treatment. Asian J Androl. 2014; 16:192–202.2. Pye SR, Huhtaniemi IT, Finn JD, Lee DM, O'Neill TW, Tajar A, et al. Late-onset hypogonadism and mortality in aging men. J Clin Endocrinol Metab. 2014; 99:1357–1366.3. Zarotsky V, Huang MY, Carman W, Morgentaler A, Singhal PK, Coffin D, et al. Systematic literature review of the risk factors, comorbidities, and consequences of hypogonadism in men. Andrology. 2014; 2:819–834.4. Corona G, Lee DM, Forti G, O'Connor DB, Maggi M, O'Neill TW, et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS). J Sex Med. 2010; 7:1362–1380.5. Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010; 363:123–135.6. Corona G, Rastrelli G, Maggi M. Diagnosis and treatment of late-onset hypogonadism: systematic review and meta-analysis of TRT outcomes. Best Pract Res Clin Endocrinol Metab. 2013; 27:557–579.7. Cai X, Tian Y, Wu T, Cao CX, Li H, Wang KJ. Metabolic effects of testosterone replacement therapy on hypogonadal men with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Asian J Androl. 2014; 16:146–152.8. Haider A, Saad F, Doros G, Gooren L. Hypogonadal obese men with and without diabetes mellitus type 2 lose weight and show improvement in cardiovascular risk factors when treated with testosterone: an observational study. Obes Res Clin Pract. 2014; 8:e339–e349.9. Saad F, Haider A, Doros G, Traish A. Long-term treatment of hypogonadal men with testosterone produces substantial and sustained weight loss. Obesity (Silver Spring). 2013; 21:1975–1981.10. Traish AM, Haider A, Doros G, Saad F. Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study. Int J Clin Pract. 2014; 68:314–329.11. Bhasin S, Pencina M, Jasuja GK, Travison TG, Coviello A, Orwoll E, et al. Reference ranges for testosterone in men generated using liquid chromatography tandem mass spectrometry in a community-based sample of healthy nonobese young men in the Framingham Heart Study and applied to three geographically distinct cohorts. J Clin Endocrinol Metab. 2011; 96:2430–2439.12. Heinemann LA. Aging Males' Symptoms scale: a standardized instrument for the practice. J Endocrinol Invest. 2005; 28(11 Suppl to no. 11):34–38.13. Yoon YS, Oh SW. Optimal waist circumference cutoff values for the diagnosis of abdominal obesity in korean adults. Endocrinol Metab. 2014; 29:418–426.14. Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999; 54:346–351.15. Heinemann LA, Saad F, Zimmermann T, Novak A, Myon E, Badia X, et al. The Aging Males' Symptoms (AMS) scale: update and compilation of international versions. Health Qual Life Outcomes. 2003; 1:15.16. Hoyos CM, Yee BJ, Phillips CL, Machan EA, Grunstein RR, Liu PY. Body compositional and cardiometabolic effects of testosterone therapy in obese men with severe obstructive sleep apnoea: a randomised placebo-controlled trial. Eur J Endocrinol. 2012; 167:531–541.17. Maggio M, Snyder PJ, De Vita F, Ceda GP, Milaneschi Y, Lauretani F, et al. Effects of transdermal testosterone treatment on inflammatory markers in elderly males. Endocr Pract. 2014; 20:1170–1177.18. Wang C, Nieschlag E, Swerdloff RS, Behre H, Hellstrom WJ, Gooren LJ, et al. ISA, ISSAM, EAU, EAA and ASA recommendations: investigation, treatment and monitoring of late-onset hypogonadism in males. Aging Male. 2009; 12:5–12.19. Yassin DJ, El Douaihy Y, Yassin AA, Kashanian J, Shabsigh R, Hammerer PG. Lower urinary tract symptoms improve with testosterone replacement therapy in men with late-onset hypogonadism: 5-year prospective, observational and longitudinal registry study. World J Urol. 2014; 32:1049–1054.20. Ko YH, Moon du G, Moon KH. Testosterone replacement alone for testosterone deficiency syndrome improves moderate lower urinary tract symptoms: one year follow-up. World J Mens Health. 2013; 31:47–52.21. Park YW, Kim SB, Kwon H, Kang HC, Cho K, Lee KI, et al. The relationship between lower urinary tract symptoms/benign prostatic hyperplasia and the number of components of metabolic syndrome. Urology. 2013; 82:674–679.22. Kwon H, Kang HC, Lee JH. Relationship between predictors of the risk of clinical progression of benign prostatic hyperplasia and metabolic syndrome in men with moderate to severe lower urinary tract symptoms. Urology. 2013; 81:1325–1329.23. Haider A, Zitzmann M, Doros G, Isbarn H, Hammerer P, Yassin A. Incidence of prostate cancer in hypogonadal men receiving testosterone therapy: observations from 5-year median followup of 3 registries. J Urol. 2015; 193:80–86.24. Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med. 2012; 366:981–990.25. Khera M, Crawford D, Morales A, Salonia A, Morgentaler A. A new era of testosterone and prostate cancer: from physiology to clinical implications. Eur Urol. 2014; 65:115–123.26. Morgentaler A. Testosterone deficiency and cardiovascular mortality. Asian J Androl. 2015; 17:26–31.27. Kelly DM, Jones TH. Testosterone and cardiovascular risk in men. Front Horm Res. 2014; 43:1–20.28. Saad F, Aversa A, Isidori AM, Zafalon L, Zitzmann M, Gooren L. Onset of effects of testosterone treatment and time span until maximum effects are achieved. Eur J Endocrinol. 2011; 165:675–685.29. Schoenfeld MJ, Shortridge E, Cui Z, Muram D. Medication adherence and treatment patterns for hypogonadal patients treated with topical testosterone therapy: a retrospective medical claims analysis. J Sex Med. 2013; 10:1401–1409.30. Donatucci C, Cui Z, Fang Y, Muram D. Long-term treatment patterns of testosterone replacement medications. J Sex Med. 2014; 11:2092–2099.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Late-onset Hypogonadism
- The Relationship between Serum Total Testosterone and Clinical Symptoms of Late-onset Hypogonadism in Aging Males
- A Manual of 2008 ISA, ISSAM, EAU, EAA and ASA Recommendations: Investigation, Treatment and Monitoring of Late-onset Hypogonadism in Males
- The Relationship between Testosterone Deficiency and Men's Health
- Physical Activity and Exercise for Men with Late Onset Hypogonadism