Ann Surg Treat Res.
2016 Mar;90(3):131-138. 10.4174/astr.2016.90.3.131.
Incidental gallbladder cancer after routine cholecystectomy: when should we suspect it preoperatively and what are predictors of patient survival?
- Affiliations
-
- 1Department of Hematology-Oncology, GangNeung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 2Department of Surgery, GangNeung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. pskys74@hanmail.net
- 3Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2155046
- DOI: http://doi.org/10.4174/astr.2016.90.3.131
Abstract
- PURPOSE
In about 1% of cases, incidental gallbladder cancers (iGBC) are found after routine cholecystectomy. The aim of this study is to compare clinical features of iGBC with benign GB disease and to evaluate factors affecting recurrence and survival.
METHODS
Between January 1998 and March 2014, 4,629 patients received cholecystectomy and 73 iGBC patients (1.6%) were identified. We compared clinical features of 4,556 benign GB disease patients with 73 iGBC patients, and evaluated operative outcomes and prognostic factors in 56 eligible patients.
RESULTS
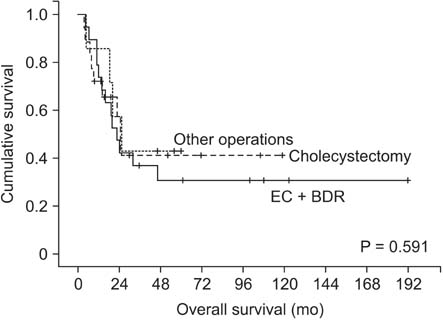
The iGBC patients were older and concomitant diseases such as hypertension and anemia were more common than benign ones. And an age of more than 65 years was the only risk factor of iGBC. Adverse prognostic factors affecting patients' survival were age over 65, advanced histology, lymph node metastasis, and lymphovascular invasion on multivariate analysis. Age over 65 years, lymph node involvement, and lymphovascular invasion were identified as unfavorable factors affecting survival in subgroup analysis of extended cholecystectomy with bile duct resection (EC with BDR, n = 22).
CONCLUSION
Prior to routine cholecystectomy, incidental GB cancer should be suspected especially in elderly patients. And advanced age, lymph node metastasis, and lymphovascular invasion are important prognostic factors in EC with BDR cohorts.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Validation of the 8th Edition of the American Joint Committee on Cancer Staging System for Gallbladder Cancer and Implications for the Follow-up of Patients without Node Dissection
You-Na Sung, Minjeong Song, Jae Hoon Lee, Ki Byung Song, Dae Wook Hwang, Chul-Soo Ahn, Shin Hwang, Seung-Mo Hong
Cancer Res Treat. 2020;52(2):455-468. doi: 10.4143/crt.2019.271.Incidental gallbladder cancer: a retrospective clinical study of 40 cases
Merih Altiok, Hanife Gülnihal Özdemir, Feyzi Kurt, Mehmet Onur Gul, Serdar Gumus
Ann Surg Treat Res. 2022;102(4):185-192. doi: 10.4174/astr.2022.102.4.185.
Reference
-
1. Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006; 56:106–130.2. Butte JM, Matsuo K, Gonen M, D'Angelica MI, Waugh E, Allen PJ, et al. Gallbladder cancer: differences in presentation, surgical treatment, and survival in patients treated at centers in three countries. J Am Coll Surg. 2011; 212:50–61.3. Shih SP, Schulick RD, Cameron JL, Lillemoe KD, Pitt HA, Choti MA, et al. Gallbladder cancer: the role of laparoscopy and radical resection. Ann Surg. 2007; 245:893–901.4. Zhang WJ, Xu GF, Zou XP, Wang WB, Yu JC, Wu GZ, et al. Incidental gallbladder carcinoma diagnosed during or after laparoscopic cholecystectomy. World J Surg. 2009; 33:2651–2656.5. Yamamoto H, Hayakawa N, Kitagawa Y, Katohno Y, Sasaya T, Takara D, et al. Unsuspected gallbladder carcinoma after laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2005; 12:391–398.6. Kwon AH, Imamura A, Kitade H, Kamiyama Y. Unsuspected gallbladder cancer diagnosed during or after laparoscopic cholecystectomy. J Surg Oncol. 2008; 97:241–245.7. Glenn F, Hays DM. The scope of radical surgery in the treatment of malignant tumors of the extrahepatic biliary tract. Surg Gynecol Obstet. 1954; 99:529–541.8. Pack GT, Miller TR, BrasfielD RD. Total right hepatic lobectomy for cancer of the gallbladder; report of three cases. Ann Surg. 1955; 142:6–16.9. Fahim RB, McDonald JR, Richards JC, Ferris DO. Carcinoma of the gallbladder: a study of its modes of spread. Ann Surg. 1962; 156:114–124.10. Pitt SC, Jin LX, Hall BL, Strasberg SM, Pitt HA. Incidental gallbladder cancer at cholecystectomy: when should the surgeon be suspicious? Ann Surg. 2014; 260:128–133.11. Lee SI, Na BG, Yoo YS, Mun SP, Choi NK. Clinical outcome for laparoscopic cholecystectomy in extremely elderly patients. Ann Surg Treat Res. 2015; 88:145–151.12. Koshenkov VP, Koru-Sengul T, Franceschi D, Dipasco PJ, Rodgers SE. Predictors of incidental gallbladder cancer in patients undergoing cholecystectomy for benign gallbladder disease. J Surg Oncol. 2013; 107:118–123.13. Manfredi S, Benhamiche AM, Isambert N, Prost P, Jouve JL, Faivre J. Trends in incidence and management of gallbladder carcinoma: a population-based study in France. Cancer. 2000; 89:757–762.14. Donohue JH. Present status of the diagnosis and treatment of gallbladder carcinoma. J Hepatobiliary Pancreat Surg. 2001; 8:530–534.15. Donohue JH, Stewart AK, Menck HR. The National Cancer Data Base report on carcinoma of the gallbladder, 1989-1995. Cancer. 1998; 83:2618–2628.16. Kayahara M, Nagakawa T, Nakagawara H, Kitagawa H, Ohta T. Prognostic factors for gallbladder cancer in Japan. Ann Surg. 2008; 248:807–814.17. Choi KS, Choi SB, Park P, Kim WB, Choi SY. Clinical characteristics of incidental or unsuspected gallbladder cancers diagnosed during or after cholecystectomy: a systematic review and metaanalysis. World J Gastroenterol. 2015; 21:1315–1323.18. Mazer LM, Losada HF, Chaudhry RM, Velazquez-Ramirez GA, Donohue JH, Kooby DA, et al. Tumor characteristics and survival analysis of incidental versus suspected gallbladder carcinoma. J Gastrointest Surg. 2012; 16:1311–1317.19. Choi SB, Han HJ, Kim CY, Kim WB, Song TJ, Suh SO, et al. Incidental gallbladder cancer diagnosed following laparoscopic cholecystectomy. World J Surg. 2009; 33:2657–2663.20. Z'graggen K, Birrer S, Maurer CA, Wehrli H, Klaiber C, Baer HU. Incidence of port site recurrence after laparoscopic cholecystectomy for preoperatively unsuspected gallbladder carcinoma. Surgery. 1998; 124:831–838.21. Lundberg O. Port site metastases after laparoscopic cholecystectomy. Eur J Surg Suppl. 2000; (585):27–30.22. Ouchi K, Mikuni J, Kakugawa Y. Organizing Committee. The 30th Annual Congress of the Japanese Society of Biliary Surgery. Laparoscopic cholecystectomy for gallbladder carcinoma: results of a Japanese survey of 498 patients. J Hepatobiliary Pancreat Surg. 2002; 9:256–260.23. Suzuki K, Kimura T, Ogawa H. Is laparoscopic cholecystectomy hazardous for gallbladder cancer? Surgery. 1998; 123:311–314.24. Yamaguchi K, Chijiiwa K, Ichimiya H, Sada M, Kawakami K, Nishikata F, et al. Gallbladder carcinoma in the era of laparoscopic cholecystectomy. Arch Surg. 1996; 131:981–984.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The appropriate surgical strategy for T1b gallbladder cancer incidentally diagnosed after a simple cholecystectomy
- When Do We Need Reoperation in Incidental Gallbladder Cancer after Laparoscopic Cholecystectomy?
- Cholelithiasis as a Risk Factor for Gallbladder Cancer
- A case of porcelain gallbladder
- Analysis of Clinical Outcome and Prognostic Factors in Patients with Gallbladder Cancer