J Korean Orthop Assoc.
2016 Feb;51(1):54-60. 10.4055/jkoa.2016.51.1.54.
Analysis of Risk Factors of Adjacent Segment Disease with Lumbar and Lumbosacral Arthrodesis for the Degenerative Lumbar Spinal Disorders
- Affiliations
-
- 1Department of Orthopedic Surgery, Chonbuk National University Medical School, Jeonju, Korea. drhwata@gmail.com
- KMID: 2154349
- DOI: http://doi.org/10.4055/jkoa.2016.51.1.54
Abstract
- PURPOSE
The objective of this study is to confirm the effects of risk factors on Adjacent Segment Disease (ASD).
MATERIALS AND METHODS
The subjects of this study were 793 patients who had degenerative lumbar spine disease and were followed-up for an average period of 7.2 years from January of 1999 to September of 2010 after undergoing spinal fusion. To confirm the risk factors, a study on patient factors, surgical factors and radiologic factors was performed.
RESULTS
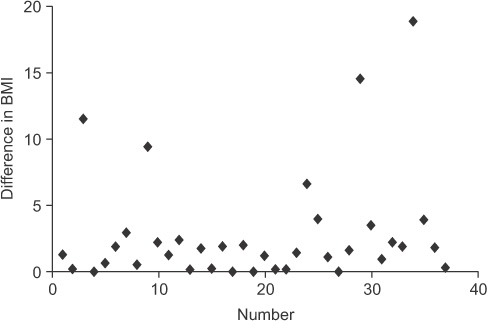
Of 793 patients, 69 patients (group A, 8.7%) underwent a secondary surgical treatment due to ASD. Age of patient, sex, bone mineral density, history of smoking and occupation were not statistically significant. Preoperative body mass index (BMI) (> or =25 kg/m2) and postoperative increase of BMI were the patient's factor in ASD (p=0.02, p<0.001). Regarding surgical factors, multilevel fusion (more than 3 levels) was higher risk in prevalence of ASD than short level fusion (p=0.01). Degeneration of intervertebral disc (p=0.01) and facet joints (p=0.02), and segmental instability (p=0.001) were also associated with the prevalence of ASD in radiologic factors.
CONCLUSION
To prevent the occurrence of ASD after lumbosacral fusion, selection of the proper level of fusion preoperatively and modifying the life style with body weight control and reduction of hypermobility after fusion surgery are essential.
MeSH Terms
Figure
Reference
-
1. Frymoyer JW, Hanley EN Jr, Howe J, Kuhlmann D, Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine (Phila Pa 1976). 1979; 4:435–440.
Article2. Booth KC, Bridwell KH, Eisenberg BA, Baldus CR, Lenke LG. Minimum 5-year results of degenerative spondylolisthesis treated with decompression and instrumented posterior fusion. Spine (Phila Pa 1976). 1999; 24:1721–1727.
Article3. Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). 1988; 13:375–377.
Article4. Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine (Phila Pa 1976). 1984; 9:574–581.
Article5. Leong JC, Chun SY, Grange WJ, Fang D. Long-term results of lumbar intervertebral disc prolapse. Spine (Phila Pa 1976). 1983; 8:793–799.
Article6. Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine (Phila Pa 1976). 1996; 21:970–981.
Article7. Kim SS, Michelsen CB. Revision surgery for failed back surgery syndrome. Spine (Phila Pa 1976). 1992; 17:957–960.
Article8. Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001; 10:314–319.
Article9. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995; 8:464–473.
Article10. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999; 90:2 Suppl. 163–169.
Article11. Chen WJ, Lai PL, Niu CC, Chen LH, Fu TS, Wong CB. Surgical treatment of adjacent instability after lumbar spine fusion. Spine (Phila Pa 1976). 2001; 26:E519–E524.
Article12. Phillips FM, Carlson GD, Bohlman HH, Hughes SS. Results of surgery for spinal stenosis adjacent to previous lumbar fusion. J Spinal Disord. 2000; 13:432–437.
Article13. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001; 26:1873–1878.
Article14. Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999; 28:215–219.
Article15. Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995; 20:1351–1358.
Article16. Ha KY, Kim KW, Park SJ, Lee YH. Changes of the adjacentunfused mobile segment after instrumental lumbar fusion: more than 5-years follow-up. J Korean Soc Spine Surg. 1998; 5:205–214.17. Shono Y, Kaneda K, Abumi K, McAfee PC, Cunningham BW. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976). 1998; 23:1550–1558.
Article18. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004; 4:190S–194S.
Article19. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004; 86:1497–1503.
Article20. Ghiselli G, Wang JC, Hsu WK, Dawson EG. L5-S1 segment survivorship and clinical outcome analysis after L4-L5 isolated fusion. Spine (Phila Pa 1976). 2003; 28:1275–1280.
Article21. Gillet P. The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech. 2003; 16:338–345.
Article22. Cho JL, Park YS, Han JH, Lee CH, Roh WI. The changes of adjacent segments after spinal fusion: follow-up more than three years after spinal fusion. J Korean Soc Spine Surg. 1998; 5:239–246.23. Lehmann TR, Spratt KF, Tozzi JE, et al. Long-term follow-up of lower lumbar fusion patients. Spine (Phila Pa 1976). 1987; 12:97–104.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Causes of Revision Arthrodesis for the Degenerative Changes at the Adjacent Segment after Lumbosacral Fusion for Degenerative Lumbar Diseases
- Preliminary Report on Usefulness of Adjacent Interspinous Stabilization using Interspinous Spacer Combined with Posterior Lumbosacral Spinal Fusion in Degenerative Lumbar Disease
- Revision Arthrodesis After Lumbar Fusion in Degenerative Lumbar Disease
- Progression of Preoperative Degeneration of the Adjacent Segmentafter Instrumented Lumbar Arthrodesis
- Surgical Treatment of Adjacent Segment Degeneration after Spinal Fusion in Degenerative Lumbar Disc Disease