J Korean Orthop Assoc.
2016 Feb;51(1):40-47. 10.4055/jkoa.2016.51.1.40.
Complications and Risk Factors of Surgery for Adult Spine Deformity
- Affiliations
-
- 1Department of Orthopedic Surgery, Eulji University Hospital, Daejeon, Korea. hjkim@eulji.ac.kr
- KMID: 2154347
- DOI: http://doi.org/10.4055/jkoa.2016.51.1.40
Abstract
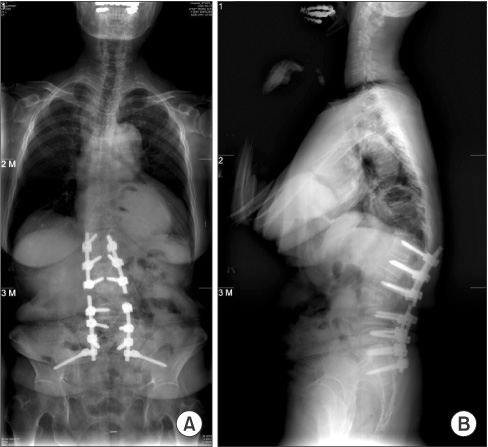
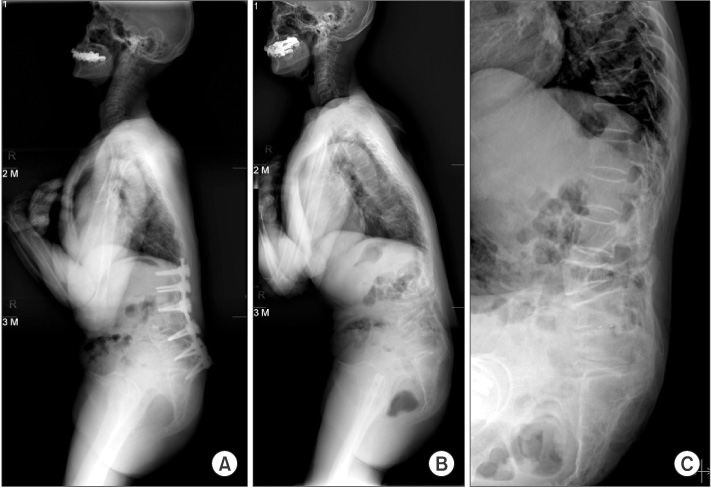
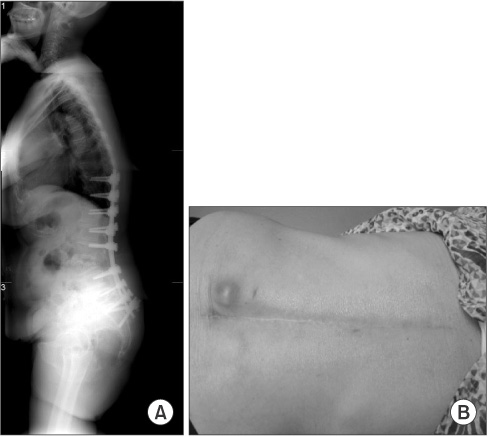
- Demand for surgical management of adult spine deformity has increased due to a recent increase in the elder population, development of surgical techniques, and increased desire for a better quality of life. More surgeries led to more and various complications. Complications of surgery for adult spine deformity have been reported from 37% to 53% depending on the types of disease, cause, and patient. This rate is higher than complications from general spine surgeries. Complications of surgery for adult spine deformity include; infection, excessive bleeding, nerve injury, pseudarthrosis, adjacent segment disease, and iliac screw complication. Factors influencing these complications include; old age, diabetes, steroid use, and osteoporosis. Proximal junctional kyphosis (PJK) is an abnormal kyphosis at the proximal level of the instrument after spine deformity surgery. Risk factors for PJK include; injury of paravertebral muscles and posterior ligament complex, over- and under-correction of coronal sagittal imbalance, age older than 55 years, and osteoporosis. There is a high risk of unexpected complications during surgery for adult spine deformity. Patients with degenerative spine sagittal imbalance are more prevalent in Korea than in Western countries. They tend to be old, have underlying diseases and osteoporosis, making them susceptible to complications related to instrumentation. Postoperative satisfaction tends to be low thus surgeons need to take care when selecting surgical methods and fusion level.
Keyword
MeSH Terms
Figure
Reference
-
1. Ayhan S, Aykac B, Yuksel S, et al. ESSG European Spine Study Group. Safety and efficacy of osteotomies in adult spinal deformity: what happens in the first year? Eur Spine J. 2015; May. 7. Published online. DOI: 10.1007/s00586-015-3981-3.
Article2. Kostuik JP, Hall BB. Spinal fusions to the sacrum in adults with scoliosis. Spine (Phila Pa 1976). 1983; 8:489–500.
Article3. Simmons ED Jr, Kowalski JM, Simmons EH. The results of surgical treatment for adult scoliosis. Spine (Phila Pa 1976). 1993; 18:718–724.
Article4. Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976). 2007; 32:2238–2244.5. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003; 85:2089–2092.
Article6. Mok JM, Cloyd JM, Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976). 2009; 34:832–839.7. Swank S, Lonstein JE, Moe JH, Winter RB, Bradford DS. Surgical treatment of adult scoliosis. A review of two hundred and twenty-two cases. J Bone Joint Surg Am. 1981; 63:268–287.
Article8. Tang H, Zhu J, Ji F, Wang S, Xie Y, Fei H. Risk factors for post-operative complication after spinal fusion and instrumentation in degenerative lumbar scoliosis patients. J Orthop Surg Res. 2014; 9:15.
Article9. Baron EM, Albert TJ. Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine (Phila Pa 1976). 2006; 31:S106–S118.
Article10. Harbrecht PJ, Garrison RN, Fry DE. Surgery in elderly patients. South Med J. 1981; 74:594–598.
Article11. Schneider SM, Veyres P, Pivot X, et al. Malnutrition is an independent factor associated with nosocomial infections. Br J Nutr. 2004; 92:105–111.
Article12. Ozkalkanli MY, Ozkalkanli DT, Katircioglu K, Savaci S. Comparison of tools for nutrition assessment and screening for predicting the development of complications in orthopedic surgery. Nutr Clin Pract. 2009; 24:274–280.
Article13. Vellas B, Lauque S, Andrieu S, et al. Nutrition assessment in the elderly. Curr Opin Clin Nutr Metab Care. 2001; 4:5–8.
Article14. Deyo RA, Hickam D, Duckart JP, Piedra M. Complications after surgery for lumbar stenosis in a veteran population. Spine (Phila Pa 1976). 2013; 38:1695–1702.
Article15. Malviya A, Walker LC, Avery P, et al. The long-term outcome of hip replacement in adults with juvenile idiopathic arthritis: the influence of steroids and methotrexate. J Bone Joint Surg Br. 2011; 93:443–448.16. Doheny MO, Sedlak CA, Estok PJ, Zeller R. Osteoporosis knowledge, health beliefs, and DXA T-scores in men and women 50 years of age and older. Orthop Nurs. 2007; 26:243–250.
Article17. Aebi M. The adult scoliosis. Eur Spine J. 2005; 14:925–948.
Article18. Donaldson MG, Cawthon PM, Lui LY, et al. Study of Osteoporotic Fractures. Estimates of the proportion of older white women who would be recommended for pharmacologic treatment by the new U.S. National Osteoporosis Foundation Guidelines. J Bone Miner Res. 2009; 24:675–680.
Article19. Lashin H, Davie MW. DXA scanning in women over 50 years with distal forearm fracture shows osteoporosis is infrequent until age 65 years. Int J Clin Pract. 2008; 62:388–393.20. Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: results from the first National Health and Nutrition Examination Survey. Int J Epidemiol. 1987; 16:537–544.
Article21. Yagi M, King AB, Boachie-Adjei O. Characterization of osteopenia/osteoporosis in adult scoliosis: does bone density affect surgical outcome? Spine (Phila Pa 1976). 2011; 36:1652–1657.22. Cloyd JM, Acosta FL Jr, Ames CP. Complications and outcomes of lumbar spine surgery in elderly people: a review of the literature. J Am Geriatr Soc. 2008; 56:1318–1327.
Article23. Guigui P, Blamoutier A. Groupe d'Etude de la Scoliose. Complications of surgical treatment of spinal deformities: a prospective multicentric study of 3311 patients. Rev Chir Orthop Reparatrice Appar Mot. 2005; 91:314–327.24. Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976). 2009; 34:1422–1428.
Article25. Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord. 1998; 11:124–128.26. Panahi P, Stroh M, Casper DS, Parvizi J, Austin MS. Operating room traffic is a major concern during total joint arthroplasty. Clin Orthop Relat Res. 2012; 470:2690–2694.
Article27. Dalstrom DJ, Venkatarayappa I, Manternach AL, Palcic MS, Heyse BA, Prayson MJ. Time-dependent contamination of opened sterile operating-room trays. J Bone Joint Surg Am. 2008; 90:1022–1025.
Article28. Cho KJ, Kim YT, Shin SH, Suk SI. Surgical treatment of adult degenerative scoliosis. Asian Spine J. 2014; 8:371–381.
Article29. Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007; 32:2232–2237.
Article30. Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D. Study Group on Scoliosis. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976). 2012; 37:693–700.31. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002; 27:776–786.32. DeWald CJ, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine (Phila Pa 1976). 2006; 31:S144–S151.33. Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. J Am Geriatr Soc. 1968; 16:622–626.
Article34. Edwards CC 2nd, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976). 2004; 29:1996–2005.
Article35. Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC 2nd, Rinella AS. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am. 2006; 88:721–728.
Article36. Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine (Phila Pa 1976). 1994; 19:1619–1627.
Article37. Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 2005; 30:1643–1649.38. Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008; 33:2179–2184.39. Hostin R, McCarthy I, O'Brien M, et al. International Spine Study Group. Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976). 2013; 38:1008–1015.
Article40. Cammarata M, Aubin CÉ, Wang X, Mac-Thiong JM. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine (Phila Pa 1976). 2014; 39:E500–E507.41. Kim YJ, Lenke LG, Bridwell KH, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine (Phila Pa 1976). 2007; 32:2731–2738.42. Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976). 2005; 30:2045–2050.43. Mendoza-Lattes S, Ries Z, Gao Y, Weinstein SL. Proximal junctional kyphosis in adult reconstructive spine surgery results from incomplete restoration of the lumbar lordosis relative to the magnitude of the thoracic kyphosis. Iowa Orthop J. 2011; 31:199–206.44. Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 2012; 37:1479–1489.45. Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine (Phila Pa 1976). 2002; 27:2350–2356.46. Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976). 2009; 34:E729–E734.47. Lau D, Clark AJ, Scheer JK, et al. SRS Adult Spinal Deformity Committee. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976). 2014; 39:2093–2102.48. Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, Hostin R. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am. 2013; 24:213–218.
Article49. Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Koester L, Hensley M. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine (Phila Pa 1976). 2010; 35:138–145.50. Kayanja MM, Schlenk R, Togawa D, Ferrara L, Lieberman I. The biomechanics of 1, 2, and 3 levels of vertebral augmentation with polymethylmethacrylate in multilevel spinal segments. Spine (Phila Pa 1976). 2006; 31:769–774.
Article51. Kim WJ, Song DG, Lee JW, et al. Proximal junctional problems in surgical treatment of lumbar degenerative sagittal imbalance patients and relevant risk factors. J Korean Soc Spine Surg. 2013; 20:156–162.
Article52. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006; 31:303–308.
Article53. Kim WJ, Chi YJ, Kang JW, et al. Complications of iliac screw in spinopelvic fixation with adult spinal deformity: complications of iliac screw in spinopelvic fixation. J Korean Soc Spine Surg. 2013; 20:113–117.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concepts and Techniques to Prevent Cervical Spine Deformity After Spine Surgery: A Narrative Review
- Minimally Invasive Spinal Surgery for Adult Spinal Deformity
- Complex Revision Surgery for Cervical Deformity or Implant Failure
- Pseudarthrosis of the Cervical Spine: Risk Factors, Diagnosis and Management
- Commentary on “Characteristics and Risk Factors of Rod Fracture Following Adult Spinal Deformity Surgery: A Systematic Review and Meta-Analysis”