J Korean Med Assoc.
2016 Feb;59(2):127-135. 10.5124/jkma.2016.59.2.127.
Reconstruction of hand
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea. drkim@korea.com
- KMID: 2153718
- DOI: http://doi.org/10.5124/jkma.2016.59.2.127
Abstract
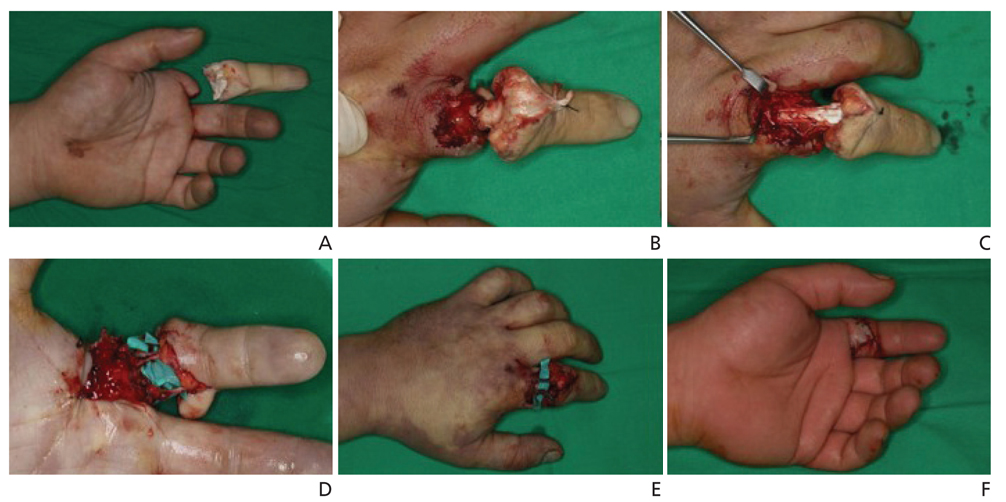
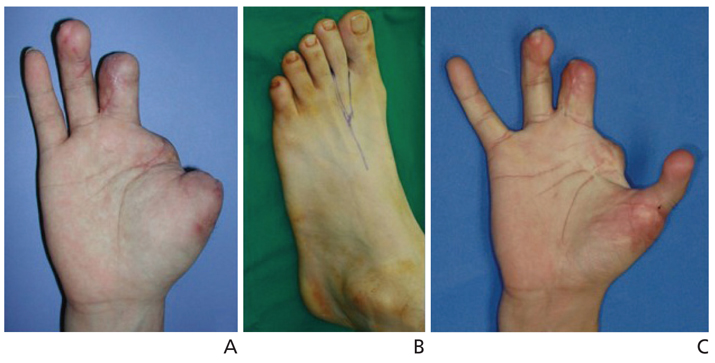
- The characteristics of hand trauma are changing due to automation of industrial facilities, improved access to health care, and the aging population. Since the inception of hand surgery as a subspecialty, hand defects have been reconstructed with the restoration of the original functionality as the primary goal. With advancement and maturation of surgical techniques, however, restoration of aesthetics also began to take hold as an important aspect of hand surgery practice. After the first successful replantation of an amputated digit, the rapid development of microsurgical techniques had a significant impact on the field of reconstructive hand surgery. In the first two decades, the success of replantation was evaluated by the survival rate for a single operator or a specialized institution. These days, however, microsurgical techniques have been widely adopted, with digital replantation possible even for infants. In addition to various local flaps, the evolution of free flaps has vastly expanded the repertoire of reconstructive options for hand surgeons. With the wide variety of free flaps available, it is possible for a severely injured hand to be salvaged and restored to its original functional and aesthetic status. In South Korea, hand surgery is becoming an established profession with a separate subspecialty certification. Hand surgery has a bright outlook, with future research directed at new biocompatible materials and novel reconstructive methods.
Keyword
MeSH Terms
Figure
Reference
-
1. Malt RA, Mckhann C. Replantation of severed arms. JAMA. 1964; 189:716–722.
Article2. Komatsu S, Tamai S. Successful replantation of a completely cut-off thumb. Plast Reconstr Surg. 1968; 42:374–377.
Article3. Hong SH, Rah SK, Park CS. Successful clinical replantation of digit and free flap transplantation with microvascular surgery. J Korean Soc Plast Reconstr Surg. 1979; 6:177–188.4. Kim JS, Yang JW, Lee DC, Ki SH, Roh SY. Challenges in fingertip replantation. Semin Plast Surg. 2013; 27:165–173.
Article5. Jeon BJ, Yang JW, Roh SY, Ki SH, Lee DC, Kim JS. Lateral nail fold incision technique for venous anastomosis in fingertip replantation. Ann Plast Surg. 2016; 76:67–71.
Article6. Roh SY, Shim WC, Lee KJ, Lee DC, Kim JS, Yang JW. Short-term strength deficit following zone 1 replantations. Arch Plast Surg. 2015; 42:614–618.
Article7. Cha GH, Woo SH, Lee DH, Seul JH. Immediate reconstruction of thumb tip injury. J Korean Soc Plast Reconstr Surg. 1991; 18:533–538.8. Woo SH. Microsurgical reconstruction of the thumb. J Korean Soc Surg Hand. 2011; 16:98–115.9. Buck-Gramcko D. Pollicization of the index finger: method and results in aplasia and hypoplasia of the thumb. J Bone Joint Surg Am. 1971; 53:1605–1617.10. Cobbett JR. Free digital transfer: report of a case of transfer of a great toe to replace an amputated thumb. J Bone Joint Surg Br. 1969; 51:677–679.11. Park JW, Byun JS, Baik BS. Reconstruction of fingers by microvascular toe transfer. J Korean Soc Plast Reconstr Surg. 1993; 20:394–409.12. Hwang SM, Ahn SM, Lim KR, Jung YH, Ryu MH. Second Toe transfer for the thumb reconstruction. J Korean Soc Surg Hand. 2009; 14:95–101.13. Jeon BJ, Yang JW, Roh SY, Ki SH, Lee DC, Kim JS. Microsurgical reconstruction of soft-tissue defects in digits. Injury. 2013; 44:356–360.
Article14. Yoo MC, Chung DW, Han JS, Ahn JH, Cha SG. Clinical analysis of free vascular flap. J Korean Orthop Assoc. 1985; 20:1145–1152.15. Lee DC, Kim JS, Ki SH, Roh SY, Yang JW, Chung KC. Partial second toe pulp free flap for fingertip reconstruction. Plast Reconstr Surg. 2008; 121:899–907.
Article16. Yang JW, Kim JS, Lee DC, Ki SH, Roh SY, Abdullah S, Tien HY. The radial artery superficial palmar branch flap: a modified free thenar flap with constant innervation. J Reconstr Microsurg. 2010; 26:529–538.
Article17. Hong JP. The use of supermicrosurgery in lower extremity reconstruction: the next step in evolution. Plast Reconstr Surg. 2009; 123:230–235.
Article18. Koshima I, Yamamoto H, Hosoda M, Moriguchi T, Orita Y, Nagayama H. Free combined composite flaps using the lateral circumflex femoral system for repair of massive defects of the head and neck regions: an introduction to the chimeric flap principle. Plast Reconstr Surg. 1993; 92:411–420.
Article19. Kim KW, Kim JS, Lee DC, Ki SH, Roh SY, Yang JW. Reconstruction of hand using anterolateral thigh fascial free flap. J Korean Soc Plast Reconstr Surg. 2009; 36:571–577.20. Park HJ, Lee DC, Kim JS, Ki SH, Roh SY, Yang JW. Tenolysis after the reconstruction of PIP joint of the finger using second toe PIP joint free flap. J Korean Soc Plast Reconstr Surg. 2009; 36:450–457.21. Squitieri L, Chung KC. A systematic review of outcomes and complications of vascularized toe joint transfer, silicone arthro-plasty, and PyroCarbon arthroplasty for posttraumatic joint reconstruction of the finger. Plast Reconstr Surg. 2008; 121:1697–1707.
Article22. Dubernard JM, Owen E, Lefrancois N, Petruzzo P, Martin X, Dawahra M, Jullien D, Kanitakis J, Frances C, Preville X, Gebu-hrer L, Hakim N, Lanzetta M, Kapila H, Herzberg G, Revillard JP. First human hand transplantation: case report. Transpl Int. 2000; 13:Suppl 1. S521–S524.
Article23. Jeon M, Lee D, Ki S, Roh S, Yang JW, Kim J. Present and future of hand surgery in Korea. J Korean Med Assoc. 2011; 54:589–593.
Article