J Korean Neurosurg Soc.
2016 Jan;59(1):37-43. 10.3340/jkns.2016.59.1.37.
Radiosurgery Compared with External Radiation Therapy as a Primary Treatment in Spine Metastasis from Hepatocellular Carcinoma : A Multicenter, Matched-Pair Study
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea. chungc@snu.ac.kr
- 2Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 3Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 4Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea.
- 5Department of Neurosurgery, Ilsan Paik Hospital, College of Medicine, Inje University, Goyang, Korea.
- 6Department of Radiation Oncology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea.
- 7Department of Nursing, College of Medicine, Chosun University, Gwangju, Korea.
- 8National Evidence-based Healthcare Collaborating Agency, Seoul, Korea.
- KMID: 2152916
- DOI: http://doi.org/10.3340/jkns.2016.59.1.37
Abstract
OBJECTIVE
The aim of this multicenter, matched-pair study was to compare the outcomes of stereotactic radiosurgery (SRS) and conventional external radiation therapy (RT) when used as a primary treatment in spine metastasis from hepatocellular carcinoma (HCC).
METHODS
From 2005 to 2012, 28 patients underwent SRS as the primary treatment in spine metastasis from HCC. Based on sex, age, number of spine metastasis, Child-Pugh classification, interval from original tumor to spine metastasis, and year of treatment, 28 patients who underwent RT were paired. Outcomes of interest were pain relief, progression free survival, toxicities, and further treatment.
RESULTS
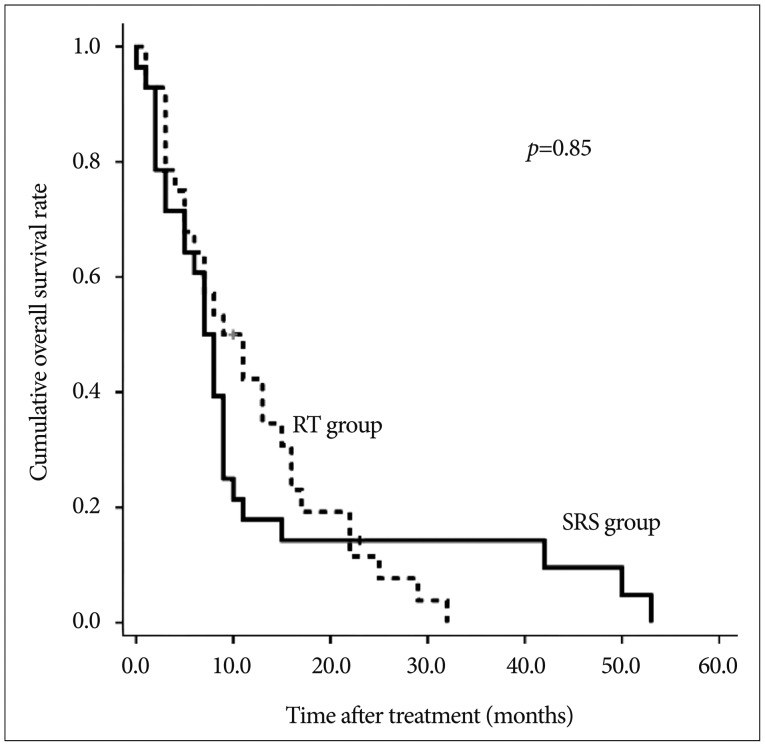
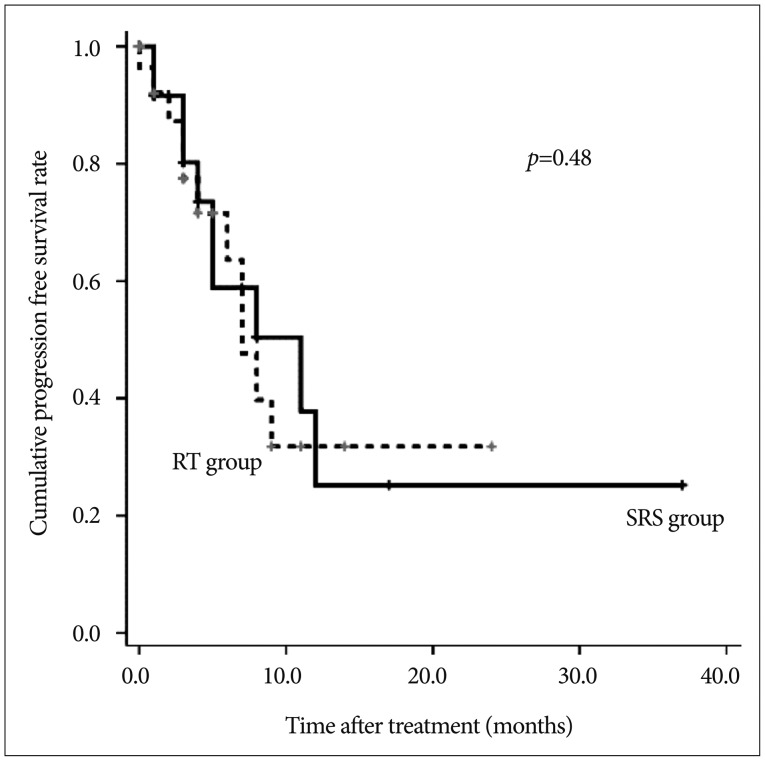
The perioperative visual analog scale (VAS) decrease was larger in SRS group than in RT group, but the difference was not significant (3.7 vs. 2.8, p=0.13). When pain medication was adjusted, the number of patients with complete (n=6 vs.3) or partial (n=12 vs.13) relief was larger in SRS group than in RT group; however, the difference was not significant (p=0.83). There was no significant difference in progression free survival (p=0.48). In SRS group, 32.1% of patients had 1 or more toxicities whereas the percentage in RT group was 63.0%, a significant difference (p=0.04). Six SRS patients and 7 RT patients received further intervention at the treated segment.
CONCLUSION
Clinical and radiological outcome were not significantly different between the two treatments. Toxicities, however, were more prevalent in the RT group.
MeSH Terms
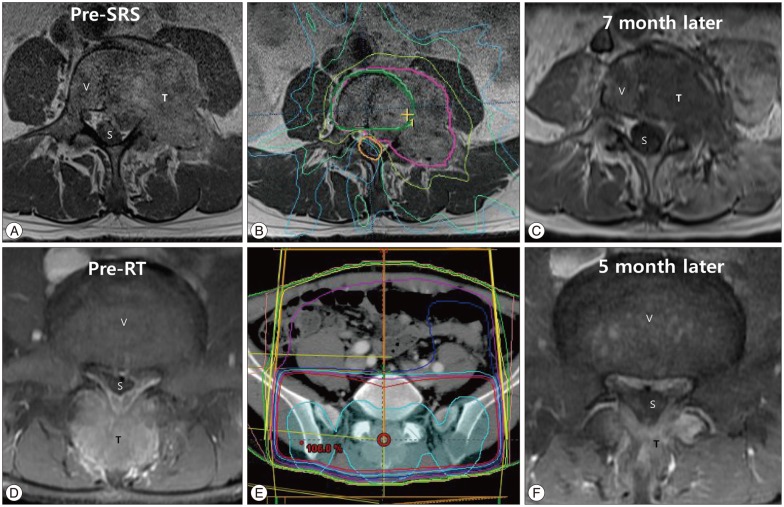
Figure
Reference
-
1. Balagamwala EH, Angelov L, Koyfman SA, Suh JH, Reddy CA, Djemil T, et al. Single-fraction stereotactic body radiotherapy for spinal metastases from renal cell carcinoma. J Neurosurg Spine. 2012; 17:556–564. PMID: 23020208.
Article2. Chang EL, Shiu AS, Mendel E, Mathews LA, Mahajan A, Allen PK, et al. Phase I/II study of stereotactic body radiotherapy for spinal metastasis and its pattern of failure. J Neurosurg Spine. 2007; 7:151–160. PMID: 17688054.
Article3. Chang UK, Cho WI, Kim MS, Cho CK, Lee DH, Rhee CH. Local tumor control after retreatment of spinal metastasis using stereotactic body radiotherapy; comparison with initial treatment group. Acta Oncol. 2012; 51:589–595. PMID: 22414095.
Article4. Chang UK, Kim MS, Han CJ, Lee DH. Clinical result of stereotactic radiosurgery for spinal metastasis from hepatocellular carcinoma : comparison with conventional radiation therapy. J Neurooncol. 2014; 119:141–148. PMID: 24803002.
Article5. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–1346. PMID: 7713792.
Article6. Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, et al. Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT) : analysis of predictive factors. Int J Radiat Oncol Biol Phys. 2012; 84:e343–e349. PMID: 22658511.7. Gagnon GJ, Henderson FC, Gehan EA, Sanford D, Collins BT, Moulds JC, et al. Cyberknife radiosurgery for breast cancer spine metastases : a matched-pair analysis. Cancer. 2007; 110:1796–1802. PMID: 17786939.
Article8. Gerszten PC, Burton SA, Ozhasoglu C, Welch WC. Radiosurgery for spinal metastases : clinical experience in 500 cases from a single institution. Spine (Phila Pa 1976). 2007; 32:193–199. PMID: 17224814.9. Gerszten PC, Mendel E, Yamada Y. Radiotherapy and radiosurgery for metastatic spine disease : what are the options, indications, and outcomes? Spine (Phila Pa 1976). 2009; 34:S78–S92. PMID: 19829280.10. Gibbs IC, Kamnerdsupaphon P, Ryu MR, Dodd R, Kiernan M, Chang SD, et al. Image-guided robotic radiosurgery for spinal metastases. Radiother Oncol. 2007; 82:185–190. PMID: 17257702.
Article11. Habermehl D, Haase K, Rieken S, Debus J, Combs SE. Defining the role of palliative radiotherapy in bone metastasis from primary liver cancer : an analysis of survival and treatment efficacy. Tumori. 2011; 97:609–613. PMID: 22158492.
Article12. Haley ML, Gerszten PC, Heron DE, Chang YF, Atteberry DS, Burton SA. Efficacy and cost-effectiveness analysis of external beam and stereotactic body radiation therapy in the treatment of spine metastases : a matched-pair analysis. J Neurosurg Spine. 2011; 14:537–542. PMID: 21314284.
Article13. Hall EJ, Brenner DJ. The radiobiology of radiosurgery : rationale for different treatment regimes for AVMs and malignancies. Int J Radiat Oncol Biol Phys. 1993; 25:381–385. PMID: 8420891.
Article14. He J, Zeng ZC, Tang ZY, Fan J, Zhou J, Zeng MS, et al. Clinical features and prognostic factors in patients with bone metastases from hepatocellular carcinoma receiving external beam radiotherapy. Cancer. 2009; 115:2710–2720. PMID: 19382203.
Article15. Kaizu T, Karasawa K, Tanaka Y, Matuda T, Kurosaki H, Tanaka S, et al. Radiotherapy for osseous metastases from hepatocellular carcinoma : a retrospective study of 57 patients. Am J Gastroenterol. 1998; 93:2167–2171. PMID: 9820391.
Article16. Lo SS, Chang EL, Ryu S, Chung H, Slotman BJ, Teh BS, et al. Best of International Stereotactic Radiosurgery Society Congress 2013 : stereotactic body radiation therapy. Part II : nonspinal tumors. Future Oncol. 2013; 9:1303–1306. PMID: 23980677.
Article17. Natsuizaka M, Omura T, Akaike T, Kuwata Y, Yamazaki K, Sato T, et al. Clinical features of hepatocellular carcinoma with extrahepatic metastases. J Gastroenterol Hepatol. 2005; 20:1781–1787. PMID: 16246200.
Article18. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden : Globocan 2000. Int J Cancer. 2001; 94:153–156. PMID: 11668491.19. Ryu S, Jin R, Jin JY, Chen Q, Rock J, Anderson J, et al. Pain control by image-guided radiosurgery for solitary spinal metastasis. J Pain Symptom Manage. 2008; 35:292–298. PMID: 18215498.
Article20. Sahgal A, Ames C, Chou D, Ma L, Huang K, Xu W, et al. Stereotactic body radiotherapy is effective salvage therapy for patients with prior radiation of spinal metastases. Int J Radiat Oncol Biol Phys. 2009; 74:723–731. PMID: 19095374.
Article21. Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, et al. Vertebral compression fracture after spine stereotactic body radiotherapy : a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol. 2013; 31:3426–3431. PMID: 23960179.
Article22. Sahgal A, Whyne CM, Ma L, Larson DA, Fehlings MG. Vertebral compression fracture after stereotactic body radiotherapy for spinal metastases. Lancet Oncol. 2013; 14:e310–e320. PMID: 23816297.
Article23. Seong J, Koom WS, Park HC. Radiotherapy for painful bone metastases from hepatocellular carcinoma. Liver Int. 2005; 25:261–265. PMID: 15780048.
Article24. Sohn MJ, Lee DJ, Yoon SW, Lee HR, Hwang YJ. The effective application of segmental image fusion in spinal radiosurgery for improved targeting of spinal tumours. Acta Neurochir (Wien). 2009; 151:231–238. discussion 238PMID: 19240972.
Article25. Sohn S, Chung CK. The role of stereotactic radiosurgery in metastasis to the spine. J Korean Neurosurg Soc. 2012; 51:1–7. PMID: 22396835.
Article26. Sohn S, Chung CK, Sohn MJ, Chang UK, Kim SH, Kim J, et al. Stereotactic radiosurgery compared with external radiation therapy as a primary treatment in spine metastasis from renal cell carcinoma : a multicenter, matched-pair study. J Neurooncol. 2014; 119:121–128. PMID: 24792488.
Article27. Tong D, Gillick L, Hendrickson FR. The palliation of symptomatic osseous metastases : final results of the Study by the Radiation Therapy Oncology Group. Cancer. 1982; 50:893–899. PMID: 6178497.
Article28. Zhang D, Xu W, Liu T, Yin H, Yang X, Wu Z, et al. Surgery and prognostic factors of patients with epidural spinal cord compression caused by hepatocellular carcinoma metastases : retrospective study of 36 patients in a single center. Spine (Phila Pa 1976). 2013; 38:E1090–E1095. PMID: 23632333.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contemporary treatment with radiosurgery for spine metastasis and spinal cord compression in 2015
- Clinical Results of Cyberknife(R) Radiosurgery for Spinal Metastases
- Stereotactic body radiotherapy for solitary spine metastasis
- The Role of Stereotactic Radiosurgery in Metastasis to the Spine
- Differences in radiotherapy application according to regional disease characteristics of hepatocellular carcinoma