Korean J Urol.
2007 Oct;48(10):1016-1021. 10.4111/kju.2007.48.10.1016.
The Relationship between the Metabolic Syndrome and the Risk of Benign Prostatic Hyperplasia: a Hospital-Based Study from a Health Screening Population
- Affiliations
-
- 1Department of Urology, Korea Cancer Center Hospital, Seoul, Korea. urodori@yahoo. co.kr
- KMID: 2139732
- DOI: http://doi.org/10.4111/kju.2007.48.10.1016
Abstract
-
PURPOSE: This case-control study was designed to investigate the possible association of the metabolic syndrome(MS) with benign prostatic hyperplasia(BPH) in healthy males.
MATERIALS AND METHODS
We reviewed the data of 702 men who had a general health check-up without significant evidence of disease. The database for health check-ups included demographic, anthropometric, serum-related and prostate-related data. The presence of the MS was determined according to the NCEP-ATPIII criteria. We compared prostate- related data between the MS and the non-MS group. Testing for linear trends and logistic regression were performed to determine whether the presence of the MS was associated with an increased risk for BPH.
RESULTS
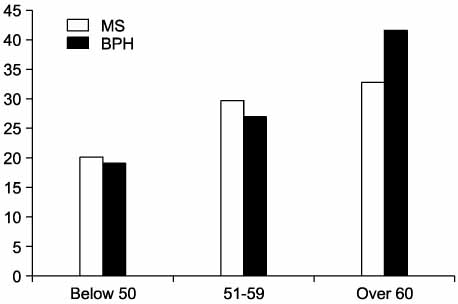
The MS was identified in 166 men(23.6%). There was an increased prevalence of both the MS and BPH along with increasing age. There was a tendency for the total prostate volume and the PSA to increase along with the an increasing number of factors related to the metabolic syndrome. In a comparison between the MS and non-MS group, there were no differences in the prostate-related variables. However, subgroup analysis in men less than 50 showed significant differences in the PSA, total volume and calculated annual growth rate. In addition, only in this group was the presence of the MS a significant risk factor for BPH(odd ratio; OR=2.21, 95% confidence interval; CI 1.28-4.75).
CONCLUSIONS
The results of this study showed a weak but significant relationship between the MS and BPH, especially in men less than 50. Further longitudinal studies with a larger patient population are required to confirm our findings.
MeSH Terms
Figure
Cited by 1 articles
-
Metabolic Syndrome and Benign Prostatic Hyperplasia: A Study Focused on the Correlation between Metabolic Syndrome Factors and Prostate Volume and Prostate-specific Antigen
Taek Hwan Jang, Jeong Hwan Son, Jae Il Kim, Seok Heun Jang
Korean J Urol. 2008;49(11):986-991. doi: 10.4111/kju.2008.49.11.986.
Reference
-
1. Lee C, Kozlowski JM, Grayhack JT. Etiology of benign prostatic hyperplasia. Urol Clin North Am. 1995. 22:237–246.2. Ozden C, Ozdal OL, Urgancioglu G, Koyuncu H, Gokkaya S, Memis A. The correlation between metabolic syndrome and prostatic growth in patients with benign prostatic hyperplasia. Eur Urol. 2007. 51:199–203.3. Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW. Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol. 2002. 168:599–604.4. Hammarsten J, Hogstedt B. Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol. 2001. 39:151–158.5. Kim JH, Shim BS, Kim JS, Hong YS. Voiding dysfunction of men is associated with metabolic syndrome. Korean J Urol. 2006. 47:257–262.6. Sohn JC, Chang HS, Kim CI. The correlation between metabolic syndrome and the prostate volume. Korean J Urol. 2007. 48:603–607.7. Park JS, Park JK. The meaning of metabolic syndrome X in patients suffering with benign prostatic hyperplasia. Korean J Urol. 2007. 48:696–700.8. Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001. 285:2486–2497.9. The Asia-Pacific perspective: redefining obesity and its treatment. WHO Regional Office for the Western Pacific/International Association for the Study of Obesity/International Obesity Task Force. 2000. Sydney: Health Communications Australia.10. Hammarsten J, Hogstedt B. Clinical, anthropometric, metabolic and insulin profile of men with fast annual growth rates of benign prostatic hyperplasia. Blood Press. 1999. 8:29–36.11. Hammarsten J, Hogstedt B, Holthuis N, Mellstrom D. Components of the metabolic syndrome-risk factors for the development of benign prostatic hyperplasia. Prostate Cancer Prostatic Dis. 1998. 1:157–162.12. Hammarsten J, Hogstedt B. Calculated fast-growing benign prostatic hyperplasia-a risk factor for developing clinical prostate cancer. Scand J Urol Nephrol. 2002. 36:330–338.13. Gupta A, Gupta S, Pavuk M, Roehrborn CG. Anthropometric and metabolic factors and risk of benign prostatic hyperplasia: a prospective cohort study of Air Force veterans. Urology. 2006. 68:1198–1205.14. Zucchetto A, Tavani A, Dal Maso L, Gallus S, Negri E, Talamini R, et al. History of weight and obesity through life and risk of benign prostatic hyperplasia. Int J Obes. 2005. 29:798–803.15. Burke JP, Rhodes T, Jacobson DJ, McGree ME, Roberts RO, Girman CJ, et al. Association of anthropometric measures with the presence and progression of benign prostatic hyperplasia. Am J Epidemiol. 2006. 164:41–46.16. Meigs JB, Mohr B, Barry MJ, Collins MM, McKinlay JB. Risk factors for clinical benign prostatic hyperplasia in a community-based population of healthy aging men. J Clin Epidemiol. 2001. 54:935. 944.17. Seitter WR, Barrett-Connor E. Cigarette smoking, obesity, and benign prostatic hypertrophy: a prospective population-based study. Am J Epidemiol. 1992. 135:500. 503.18. Gann PH, Hennekens CH, Longcope C, Verhoek-Oftedahl W, Grodstein F, Stampfer MJ. A prospective study of plasma hormone levels, nonhormonal factors, and development of benign prostatic hyperplasia. Prostate. 1995. 26:40–49.19. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.20. Park HK, Lee KS, KCHAR , Han BK, Jeong SJ, Hong SK, et al. The relationship between metabolic syndrome and voiding dysfunction in aged men of local community. Korean J Urol. 2006. 47:Suppl 2. 141. abstract P-29.21. Peehl DM, Cohen P, Rosenfeld RG. The role of insulin-like growth factors in prostatic biology. J Androl. 1996. 17:2–4.22. Lym YL, Hwang SW, Shim HJ, Oh EH, Chang YS, Cho BL. Prevalence and risk factors of the metabolic syndrome as defined by NCEP-ATP III. J Korean Acad Fam Med. 2003. 24:135–143.23. Kim BS. Prevalence of metabolic syndrome for Koreans. Korean J Health Promot Dis. 2002. 2:17–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the editor: Impact of metabolic syndrome on response to medical treatment of benign prostatic hyperplasia
- The Correlation between Metabolic Syndrome and the Prostate Volume
- The Relating Factors of Metabolic Syndrome to Benign Prostatic Hyperplasia
- Metabolic Syndrome and Benign Prostatic Hyperplasia: Evidence of a Potential Relationship, Hypothesized Etiology, and Prevention
- Association of Metabolic Syndrome and Benign Prostate Enlargement in Young Korean Males