J Korean Assoc Pediatr Surg.
2015 Dec;21(2):17-23. 10.13029/jkaps.2015.21.2.17.
Surgical Treatment of Difficult Cervicofacial Lymphangioma in Children
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jm0815.seo@samsung.com
- 2Department of Plastic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2133784
- DOI: http://doi.org/10.13029/jkaps.2015.21.2.17
Abstract
- PURPOSE
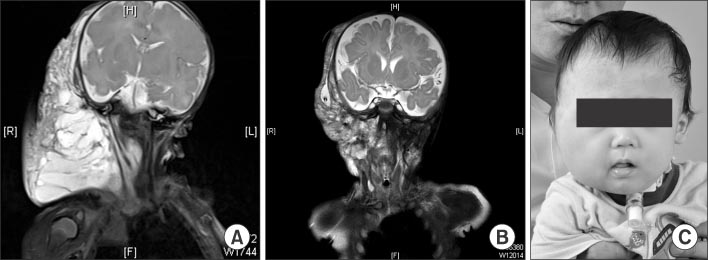
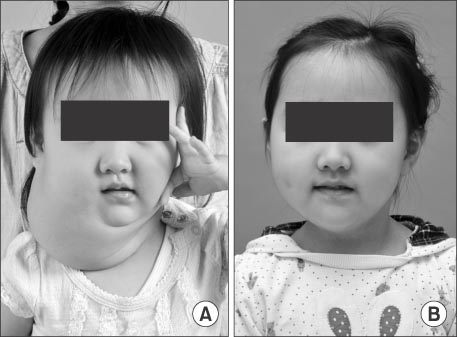
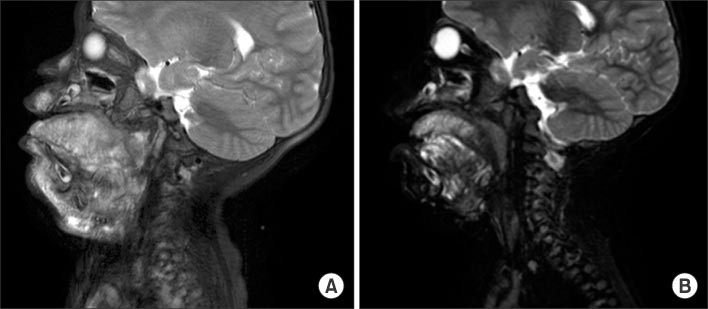
Cervical lymphangiomas are rare lymphovascular malformations arising in the neck, which form huge fluid-containing cysts. Treatment of the malformation consists of surgery and sclerotherapy. However, the optimal approach is still controversial. Here, we describe a series of cervical lymphangiomas which have been treated with surgical approaches.
METHODS
We retrospectively investigated the medical records of 82 patients who had been diagnosed with cervicofacial lymphangioma from 2001 to 2012 in our center. A closed suction drainage with negative pressure was placed on the operative lesion following excision to prevent reaccumulation of lymphatic fluid and the drainage tube was removed after injecting OK-432 through the tube.
RESULTS
Twelve patients underwent surgical excision of cervical lymphangioma. The median patient age was 3 months at the time of the operation. The patients have been followed-up over a period of 34 months. When lesions were located near vital organs such as the trachea or carotid artery or did not respond to repetitive OK-432 injections, surgical treatment might bring good outcomes. However, swallowing difficulty, lip palsy, or dyslalia due to adjacent nerve damage temporarily appeared as postoperative complications. Five children had tracheostomy due to tracheal or subglottic stenosis and 2 patients had gastrostomy due to aspiration while they eat after surgery.
CONCLUSION
Surgery for cervicofacial lymphangioma should be conducted carefully in selective cases. A well thought-out surgical plan with a multidisciplinary surgical team approach and placement of closed suction drainage tube after surgery and adjuvant OK-432 sclerotherapy through drainage tube seem to be helpful for good outcome.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Treatment Experience of Lymphatic Malformations in Pediatric Patients
Jae Ha Park, So Hyun Nam
J Korean Assoc Pediatr Surg. 2018;24(1):14-19. doi: 10.13029/jkaps.2018.24.1.14.Abdominal Lymphatic Malformation in Children
Sangho Lee, Jinyoung Park
Adv Pediatr Surg. 2018;24(2):60-67. doi: 10.13029/aps.2018.24.2.60.
Reference
-
1. Poldervaart MT, Breugem CC, Speleman L, Pasmans S. Treatment of lymphatic malformations with OK-432 (Picibanil): review of the literature. J Craniofac Surg. 2009; 20:1159–1162.2. Weiss SW, Goldblum JR, Enzinger FM. Enzinger and Weiss's soft tissue tumors. 5th ed. Philadelphia, PA: Mosby Elsevier;2008.3. Luzzatto C, Midrio P, Tchaprassian Z, Guglielmi M. Sclerosing treatment of lymphangiomas with OK-432. Arch Dis Child. 2000; 82:316–318.4. Mitsukawa N, Satoh K. New treatment for cystic lymphangiomas of the face and neck: cyst wall rupture and cyst aspiration combined with sclerotherapy. J Craniofac Surg. 2012; 23:1117–1119.5. Churchill P, Otal D, Pemberton J, Ali A, Flageole H, Walton JM. Sclerotherapy for lymphatic malformations in children: a scoping review. J Pediatr Surg. 2011; 46:912–922.6. Okazaki T, Iwatani S, Yanai T, Kobayashi H, Kato Y, Marusasa T, et al. Treatment of lymphangioma in children: our experience of 128 cases. J Pediatr Surg. 2007; 42:386–389.7. Kim MG, Kim SG, Lee JH, Eun YG, Yeo SG. The therapeutic effect of OK-432 (picibanil) sclerotherapy for benign neck cysts. Laryngoscope. 2008; 118:2177–2181.8. Yoo JC, Ahn Y, Lim YS, Hah JH, Kwon TK, Sung MW, et al. OK-432 sclerotherapy in head and neck lymphangiomas: long-term follow-up result. Otolaryngol Head Neck Surg. 2009; 140:120–123.9. Adams MT, Saltzman B, Perkins JA. Head and neck lymphatic malformation treatment: a systematic review. Otolaryngol Head Neck Surg. 2012; 147:627–639.10. Kim SY, Lee S, Seo JM, Lim SY. Postoperative adjuvant OK-432 sclerotherapy for treatment of cervicofacial lymphatic malformations: an outcomes comparison. Int J Pediatr Otorhinolaryngol. 2015; 79:570–575.11. Chakravarti A, Bhargava R. Lymphangioma circumscriptum of the tongue in children: successful treatment using intralesional bleomycin. Int J Pediatr Otorhinolaryngol. 2013; 77:1367–1369.12. Hirose S, Harrison MR. The ex utero intrapartum treatment (EXIT) procedure. Semin Neonatol. 2003; 8:207–214.13. Leva E, Pansini L, Fava G, Maestri L, Pansini A, Selvaggio G. The role of the surgeon in the case of a giant neck mass in the EXIT procedure. J Pediatr Surg. 2005; 40:748–750.14. Stevens GH, Schoot BC, Smets MJ, Kremer B, Manni JJ, Gavilanes AW, et al. The ex utero intrapartum treatment (EXIT) procedure in fetal neck masses: a case report and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2002; 100:246–250.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphangioma in children
- Cystic Lymphangioma of Rectum-A Case Report and Review of Literature
- Retroperitoneal cystic lymphangioma in an aged man: report of a case and review of the literature
- A Case of Cystic Lymphangioma of the Scrotum and Retroperitoneum
- Comments to "A Acquired Lymphangioma Circumscriptum of the Nipple Areola"