Yonsei Med J.
2014 Jul;55(4):1115-1122. 10.3349/ymj.2014.55.4.1115.
Estimation of Gastrocnemius Muscle Volume Using Ultrasonography in Children with Spastic Cerebral Palsy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Severance Hospital, Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. werch@yuhs.ac
- KMID: 2130841
- DOI: http://doi.org/10.3349/ymj.2014.55.4.1115
Abstract
- PURPOSE
This study aimed to investigate useful parameters for estimating gastrocnemius (GCM) muscle volume (MV) using ultrasonography (US) and anthropometry in children with spastic cerebral palsy (CP).
MATERIALS AND METHODS
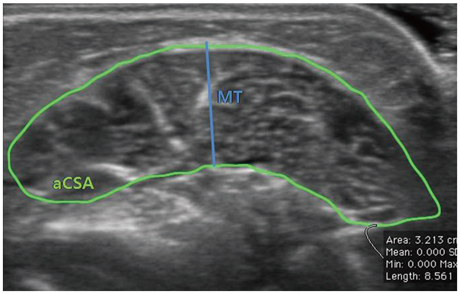
Eighteen legs from nine children with spastic CP aged 2 to 6 years were investigated in this study. Tibial length (TL) of each leg was measured and muscle thickness (MT) and anatomical cross-sectional area (aCSA) of GCM muscles were assessed using US. The volume of the GCM was measured by magnetic resonance imaging (MRI) scans. The relationship of TL, MT, and aCSA with MV measured by MRI was investigated. Simple and multiple regression analyses were performed to establish muscle volume prediction equations.
RESULTS
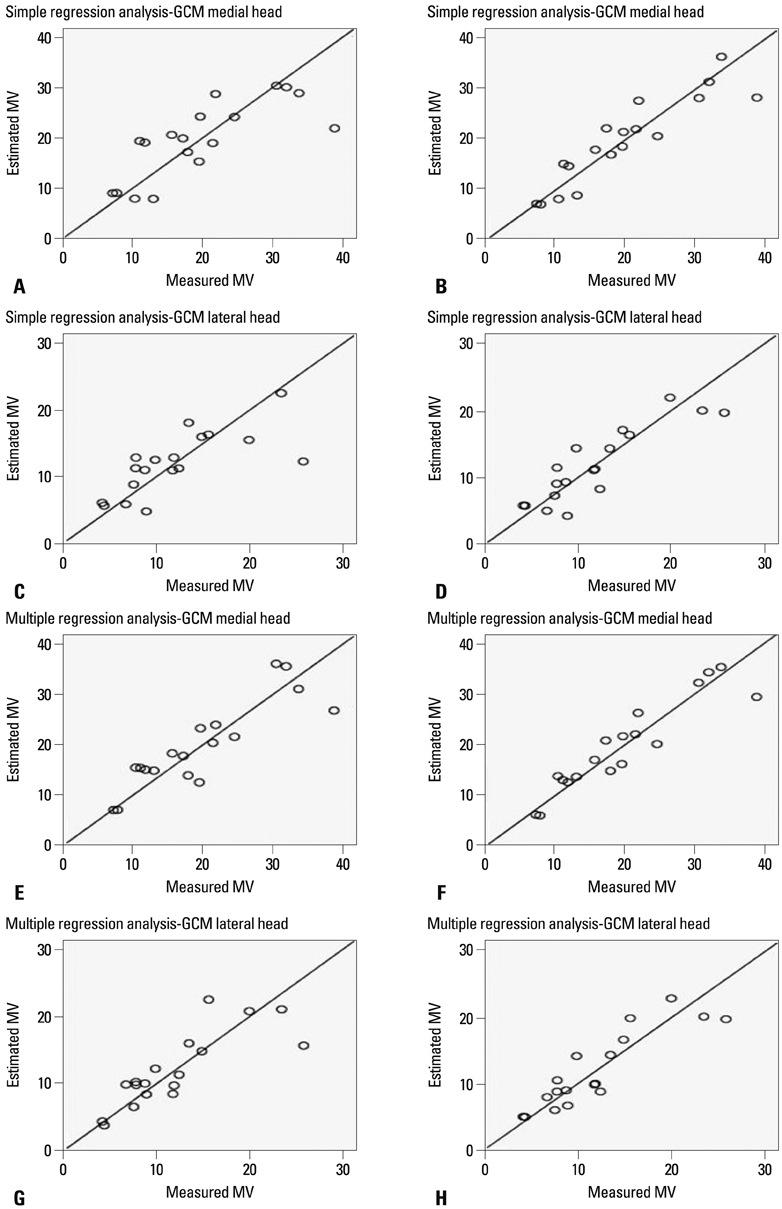
Resting MT, aCSA, and TL were highly related to MV of both medial and lateral head of GCM determined by MRI. The MV prediction equation based on simple regression analysis resulted in r2 values ranging from 0.591 to 0.832 (p<0.05). The r2 values were higher using aCSA as independent variable than using MT. The MV prediction equation based on multiple regression analysis resulted in r2 values ranging from 0.779 to 0.903 (p<0.05). However, the relatively high standard error of the estimate values ranged from 18.0-33.6% on simple regression and 15.5-25.6% on multiple regression. The contribution of aCSA was higher than that of MT for predicting MV of GCM.
CONCLUSION
Our study demonstrated the suitability of US assessment of aCSA and MT combined with TL for estimating MV of GCM in children with spastic CP and showed that aCSA is more useful parameter than MT.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Relationship Between Functional Level and Muscle Thickness in Young Children With Cerebral Palsy
Yeo Reum Choe, Joo Sup Kim, Kee Hoon Kim, Tae Im Yi
Ann Rehabil Med. 2018;42(2):286-295. doi: 10.5535/arm.2018.42.2.286.
Reference
-
1. Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005; 47:571–576.
Article2. Barrett RS, Lichtwark GA. Gross muscle morphology and structure in spastic cerebral palsy: a systematic review. Dev Med Child Neurol. 2010; 52:794–804.
Article3. Barber L, Hastings-Ison T, Baker R, Barrett R, Lichtwark G. Medial gastrocnemius muscle volume and fascicle length in children aged 2 to 5 years with cerebral palsy. Dev Med Child Neurol. 2011; 53:543–548.
Article4. Fukunaga T, Miyatani M, Tachi M, Kouzaki M, Kawakami Y, Kanehisa H. Muscle volume is a major determinant of joint torque in humans. Acta Physiol Scand. 2001; 172:249–255.
Article5. Fukunaga T, Ito M, Ichinose Y, Kuno S, Kawakami Y, Fukashiro S. Tendinous movement of a human muscle during voluntary contractions determined by real-time ultrasonography. J Appl Physiol (1985). 1996; 81:1430–1433.
Article6. Blazevich AJ, Coleman DR, Horne S, Cannavan D. Anatomical predictors of maximum isometric and concentric knee extensor moment. Eur J Appl Physiol. 2009; 105:869–878.
Article7. Gadeberg P, Andersen H, Jakobsen J. Volume of ankle dorsiflexors and plantar flexors determined with stereological techniques. J Appl Physiol (1985). 1999; 86:1670–1675.
Article8. Akagi R, Takai Y, Ohta M, Kanehisa H, Kawakami Y, Fukunaga T. Muscle volume compared to cross-sectional area is more appropriate for evaluating muscle strength in young and elderly individuals. Age Ageing. 2009; 38:564–569.
Article9. Pitcher CA, Elliott CM, Williams SA, Licari MK, Kuenzel A, Shipman PJ, et al. Childhood muscle morphology and strength: alterations over six months of growth. Muscle Nerve. 2012; 46:360–366.
Article10. McBurney H, Taylor NF, Dodd KJ, Graham HK. A qualitative analysis of the benefits of strength training for young people with cerebral palsy. Dev Med Child Neurol. 2003; 45:658–663.
Article11. Ohata K, Tsuboyama T, Ichihashi N, Minami S. Measurement of muscle thickness as quantitative muscle evaluation for adults with severe cerebral palsy. Phys Ther. 2006; 86:1231–1239.
Article12. McNee AE, Gough M, Morrissey MC, Shortland AP. Increases in muscle volume after plantarflexor strength training in children with spastic cerebral palsy. Dev Med Child Neurol. 2009; 51:429–435.
Article13. Tok F, Ozçakar L, Safaz I, Alaca R. Effects of botulinum toxin-A on the muscle architecture of stroke patients: the first ultrasonographic study. J Rehabil Med. 2011; 43:1016–1019.
Article14. Heymsfield SB, McManus C, Smith J, Stevens V, Nixon DW. Anthropometric measurement of muscle mass: revised equations for calculating bone-free arm muscle area. Am J Clin Nutr. 1982; 36:680–690.
Article15. Rice CL, Cunningham DA, Paterson DH, Lefcoe MS. A comparison of anthropometry with computed tomography in limbs of young and aged men. J Gerontol. 1990; 45:M175–M179.
Article16. Reeves ND, Narici MV, Maganaris CN. Effect of resistance training on skeletal muscle-specific force in elderly humans. J Appl Physiol (1985). 2004; 96:885–892.
Article17. Ahtiainen JP, Hoffren M, Hulmi JJ, Pietikäinen M, Mero AA, Avela J, et al. Panoramic ultrasonography is a valid method to measure changes in skeletal muscle cross-sectional area. Eur J Appl Physiol. 2010; 108:273–279.
Article18. Linney AD, Deng J. Three-dimensional morphometry in ultrasound. Proc Inst Mech Eng H. 1999; 213:235–245.
Article19. Fenster A, Downey DB. Three-dimensional ultrasound imaging. Annu Rev Biomed Eng. 2000; 2:457–475.
Article20. Barber L, Barrett R, Lichtwark G. Validation of a freehand 3D ultrasound system for morphological measures of the medial gastrocnemius muscle. J Biomech. 2009; 42:1313–1319.
Article21. Moreau NG, Teefey SA, Damiano DL. In vivo muscle architecture and size of the rectus femoris and vastus lateralis in children and adolescents with cerebral palsy. Dev Med Child Neurol. 2009; 51:800–806.
Article22. Mohagheghi AA, Khan T, Meadows TH, Giannikas K, Baltzopoulos V, Maganaris CN. In vivo gastrocnemius muscle fascicle length in children with and without diplegic cerebral palsy. Dev Med Child Neurol. 2008; 50:44–50.
Article23. Infantolino BW, Gales DJ, Winter SL, Challis JH. The validity of ultrasound estimation of muscle volumes. J Appl Biomech. 2007; 23:213–217.
Article24. Bandholm T, Sonne-Holm S, Thomsen C, Bencke J, Pedersen SA, Jensen BR. Calf muscle volume estimates: implications for botulinum toxin treatment? Pediatr Neurol. 2007; 37:263–269.
Article25. Esformes JI, Narici MV, Maganaris CN. Measurement of human muscle volume using ultrasonography. Eur J Appl Physiol. 2002; 87:90–92.
Article26. Miyatani M, Kanehisa H, Kuno S, Nishijima T, Fukunaga T. Validity of ultrasonograph muscle thickness measurements for estimating muscle volume of knee extensors in humans. Eur J Appl Physiol. 2002; 86:203–208.
Article27. Miyatani M, Kanehisa H, Ito M, Kawakami Y, Fukunaga T. The accuracy of volume estimates using ultrasound muscle thickness measurements in different muscle groups. Eur J Appl Physiol. 2004; 91:264–272.
Article28. Miyatani M, Kanehisa H, Fukunaga T. Validity of bioelectrical impedance and ultrasonographic methods for estimating the muscle volume of the upper arm. Eur J Appl Physiol. 2000; 82:391–396.
Article29. Choi WH, Song CW, Kim YB, Ha CS, Yang GH, Woo HD, et al. Skeletal muscle atrophy induced by intramuscular repeated dose of botulinum toxin type A in rats. Drug Chem Toxicol. 2007; 30:217–227.
Article30. Cosgrove AP, Corry IS, Graham HK. Botulinum toxin in the management of the lower limb in cerebral palsy. Dev Med Child Neurol. 1994; 36:386–396.
Article31. Williams SA, Reid S, Elliott C, Shipman P, Valentine J. Muscle volume alterations in spastic muscles immediately following botulinum toxin type-A treatment in children with cerebral palsy. Dev Med Child Neurol. 2013; 55:813–820.
Article32. Bénard MR, Becher JG, Harlaar J, Huijing PA, Jaspers RT. Anatomical information is needed in ultrasound imaging of muscle to avoid potentially substantial errors in measurement of muscle geometry. Muscle Nerve. 2009; 39:652–665.
Article33. e Lima KM, da Matta TT, de Oliveira LF. Reliability of the rectus femoris muscle cross-sectional area measurements by ultrasonography. Clin Physiol Funct Imaging. 2012; 32:221–226.
Article34. Lampe R, Grassl S, Mitternacht J, Gerdesmeyer L, Gradinger R. MRT-measurements of muscle volumes of the lower extremities of youths with spastic hemiplegia caused by cerebral palsy. Brain Dev. 2006; 28:500–506.
Article35. Williams SA, Elliott C, Valentine J, Gubbay A, Shipman P, Reid S. Combining strength training and botulinum neurotoxin intervention in children with cerebral palsy: the impact on muscle morphology and strength. Disabil Rehabil. 2013; 35:596–605.
Article36. Riad J, Modlesky CM, Gutierrez-Farewik EM, Broström E. Are muscle volume differences related to concentric muscle work during walking in spastic hemiplegic cerebral palsy? Clin Orthop Relat Res. 2012; 470:1278–1285.
Article37. Fry NR, Gough M, McNee AE, Shortland AP. Changes in the volume and length of the medial gastrocnemius after surgical recession in children with spastic diplegic cerebral palsy. J Pediatr Orthop. 2007; 27:769–774.
Article38. Morse CI, Thom JM, Reeves ND, Birch KM, Narici MV. In vivo physiological cross-sectional area and specific force are reduced in the gastrocnemius of elderly men. J Appl Physiol (1985). 2005; 99:1050–1055.
Article39. Masuda K, Kikuhara N, Takahashi H, Yamanaka K. The relationship between muscle cross-sectional area and strength in various isokinetic movements among soccer players. J Sports Sci. 2003; 21:851–858.
Article40. Bemben MG. Use of diagnostic ultrasound for assessing muscle size. J Strength Cond Res. 2002; 16:103–108.
Article41. Noorkoiv M, Nosaka K, Blazevich AJ. Assessment of quadriceps muscle cross-sectional area by ultrasound extended-field-of-view imaging. Eur J Appl Physiol. 2010; 109:631–639.
Article42. Howe TE, Oldham JA. The reliability of measuring quadriceps cross-sectional area with compound B ultrasound scanning. Physiother Res Int. 1996; 1:112–126.
Article43. Morse CI, Degens H, Jones DA. The validity of estimating quadriceps volume from single MRI cross-sections in young men. Eur J Appl Physiol. 2007; 100:267–274.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Change of Dynamic Gastrocnemius Length after the Block of Spastic Gastrocnemius Muscle in Cerebral Palsy
- Gastrocnemius Architecture in Patients with Spastic Cerebral Palsy
- Therapeutic Effect of Extracorporeal Shock Wave Therapy According to Treatment Session on Gastrocnemius Muscle Spasticity in Children With Spastic Cerebral Palsy: A Pilot Study
- Ultrasonographic Measurement of Gastrocnemius Muscle Thickness in Spastic Cerebral Palsy and Influencing Factors
- The Change of Intrinsic Stiffness in Gastrocnemius after Intensive Rehabilitation with Botulinum Toxin A Injection in Spastic Diplegic Cerebral Palsy