J Korean Ophthalmol Soc.
2015 May;56(5):776-779. 10.3341/jkos.2015.56.5.776.
A Case of Eccrine Spiradenoma of the Eyelid
- Affiliations
-
- 1Saevit Eye Hospital, Goyang, Korea. lkw740306@hanmail.net
- 2Department of Ophthalmology and Visual Science, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Pathology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2121179
- DOI: http://doi.org/10.3341/jkos.2015.56.5.776
Abstract
- PURPOSE
To report a case of eccrine spiradenoma that presented as an eyelid nodule.
CASE SUMMARY
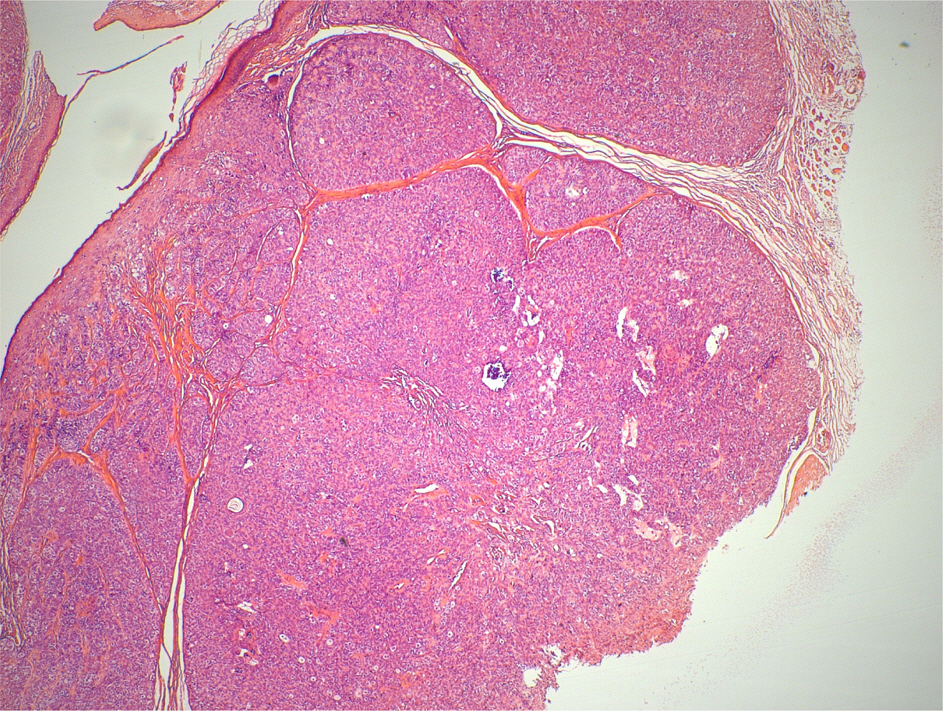
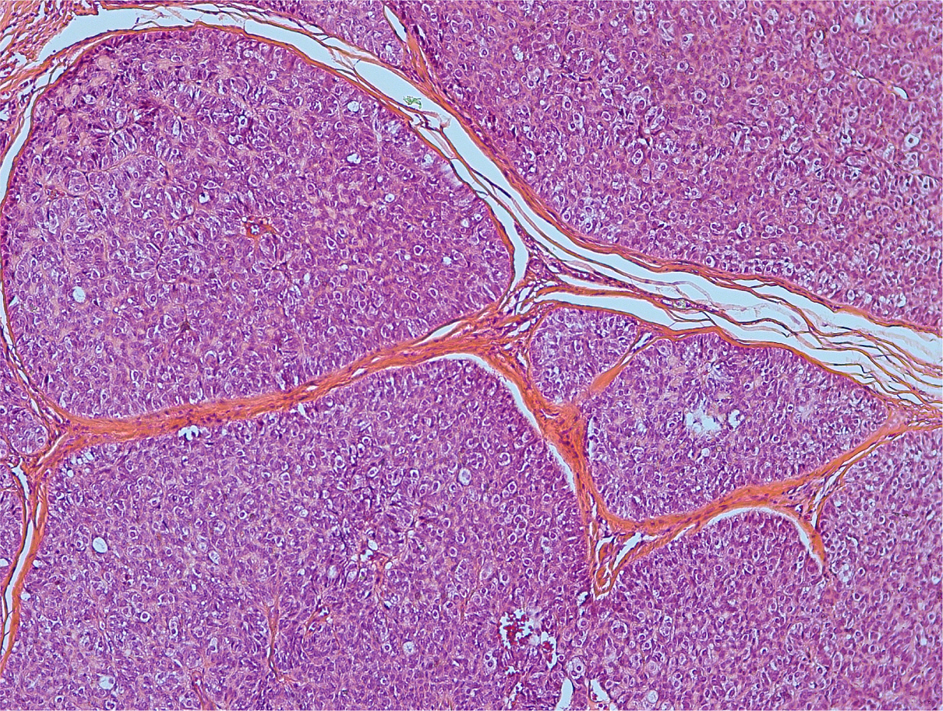
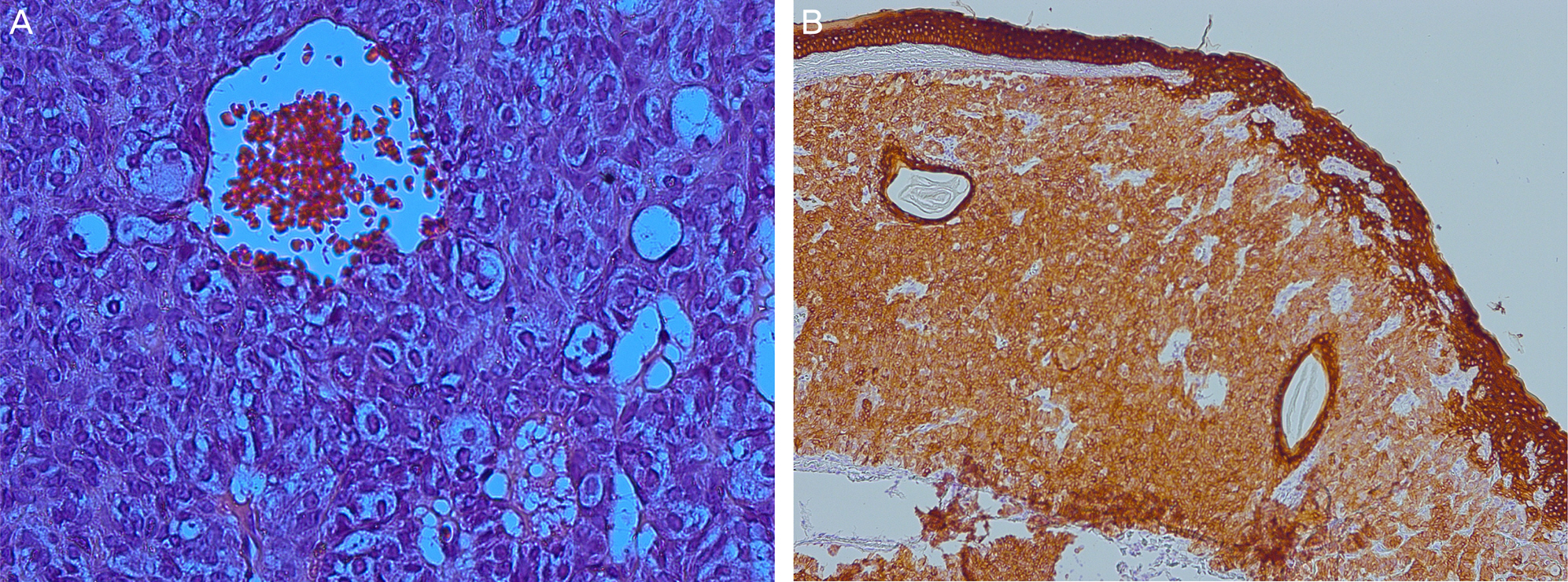
A 61-year-old female presented with a mass in the right upper lid margin; the onset time was unknown. An ophthalmic examination revealed no abnormalities except the eyelid nodule. The nodule was 3 mm in size with a firm, smooth surface and light pinkish color, and was located near the lid margin. Excision and biopsy of the nodule was performed. The pathological findings of the specimen obtained showed islands of 2 types of lobular cells. Larger, paler cells were grouped around the central area, darker and smaller cells on the periphery. These findings were compatible with eccrine spiradenoma.
CONCLUSIONS
Eccrine spiradenoma should be considered a differential diagnosis of a solitary eyelid tumor.
Keyword
Figure
Reference
-
References
1. Kersting DW, Helwig EB. Eccrine spiradenoma. AMA Arch Derm. 1956; 73:199–227.
Article2. Wright S, Ryan J. Multiple familial eccrine spiradenoma with cylindroma. Acta Derm Venereol. 1990; 70:79–82.3. Ekmekci TR, Koslu A, Sakiz D. Congenital blaschkoid eccrine spiradenoma on the face. Eur J Dermatol. 2005; 15:73–4.4. Scheinfeld NS, Tarlow MM, Burgin S. Blaschkoid eccrine spiradenomas. Cutis. 2002; 70:73–5.5. Amann J, Spraul CW, Mattfeld T, Lang GK. Eccrine spiradenoma of the eyelid. Klin Monbl Augenheilkd. 1999; 214:53–4.6. Buiuc S, Savin R, Beşchea G, et al. Eccrine spiradenoma of the eyelids. Rev Chir Oncol Radiol O R L Oftalmol Stomatol Ser Oftalmol. 1979; 23:225–6.7. Ahluwalia BK, Khurana AK, Chugh AD, Mehtani VG. Eccrine spiradenoma of eyelid: case report. Br J Ophthalmol. 1986; 70:580–3.
Article8. Kanitakis J, Schmitt D, Thivolet J. Contribution of monoclonal an-tibody D 47 in the study of sweat gland pathology. Ann Pathol. 1985; 5:19–27.9. Gupta S, Radotra BD, Kaur I, et al. Multiple linear eccrine spiradenomas with eyelid involvement. J Eur Acad Dermatol Venereol. 2001; 15:163–6.
Article10. Ekmekci TR, Koslu A, Sakiz D. Congenital blaschkoid eccrine spiradenoma on the face. Eur J Dermatol. 2005; 15:73–4.11. Cooper PH, Frierson HF Jr, Morrison AG. Malignant trans-formation of eccrine spiradenoma. Arch Dermatol. 1985; 121:1445–8.
Article12. Kim MH, Cho E, Lee JD, Cho SH. Giant vascular eccrine spiradenoma. Ann Dermatol. 2011; 23(Suppl 2):S197–200.
Article