Effects of Early Surgical Exploration in Suspected Barotraumatic Perilymph Fistulas
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. whchung@skku.edu
- KMID: 2117500
- DOI: http://doi.org/10.3342/ceo.2012.5.2.74
Abstract
OBJECTIVES
Treatment of traumatic perilymph fistula (PLF) remains controversial between surgical repair and conservative therapy. The aim of this study is to analyze the outcomes of early surgical exploration in suspected barotraumatic PLF.
METHODS
Nine patients (10 cases) who developed sudden sensorineural hearing loss and dizziness following barotrauma and underwent surgical exploration with the clinical impression of PLF were enrolled. Types of antecedent trauma, operative findings, control of dizziness after surgery, postoperative hearing outcomes, and relations to the time interval between traumatic event and surgery were assessed retrospectively.
RESULTS
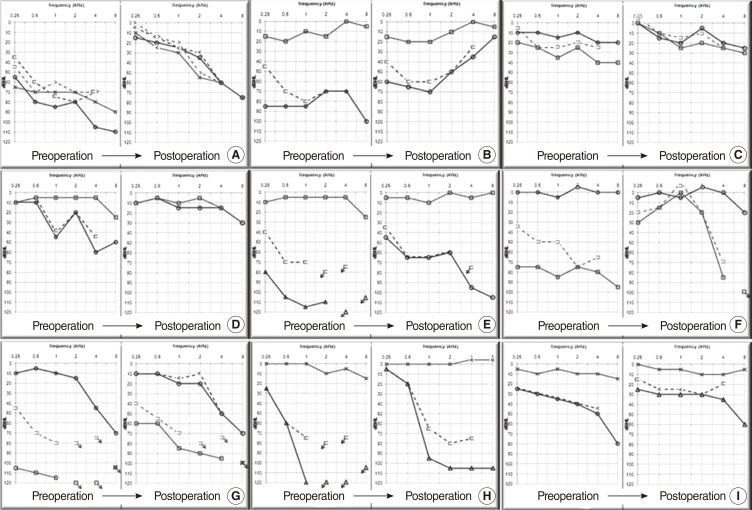
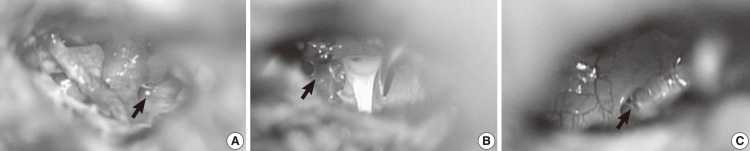
All patients had sudden or progressive hearing loss and dizziness following trauma. Types of barotrauma were classified by the origin of the trauma: 4 external (car accident, slap injury) and 6 internal traumas (lifting, nasal blowing, straining). Surgical exploration was performed whenever PLF was suspected with the time interval of 2 to 47 days after the trauma. The possible evidence of PLF was found during surgery in 9 cases: a fibrous web around the oval window (n=3), fluid collection in the round window (RW; n=6) and bulging of the RW pseudomembrane (n=1). In every patient, vestibular symptoms disappeared immediately after surgery. The hearing was improved with a mean gain of 27.0+/-14.9 dB. When the surgical exploration was performed as early as less than 10 days after the trauma, serviceable hearing (< or =40 dB) was obtained in 4 out of 7 cases (57.1%).
CONCLUSION
Sudden or progressive sensorineural hearing loss accompanied by dizziness following barotrauma should prompt consideration of PLF. Early surgical exploration is recommended to improve hearing and vestibular symptoms.
Keyword
Figure
Cited by 3 articles
-
Two Cases of Recurred Vertigo Following Perilymphatic Oval Window Fistula Repair
Hack Jung Kim, Won-Ho Chung
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(2):103-107. doi: 10.3342/kjorl-hns.2020.00206.Two Cases of Idiopathic Progressive Sensorineural Hearing Loss with Positional Nystagmus in Postpartum Period: Possible Spontaneous Perilymph Fistula?
Minhae Park, Hee Jung Kim, Won-Ho Chung
Korean J Otorhinolaryngol-Head Neck Surg. 2021;64(8):585-591. doi: 10.3342/kjorl-hns.2020.00668.Significance of Pseudo-Conductive Hearing Loss and Positional Nystagmus for Perilymphatic Fistula: Are They Related to Third-Window Effects?
Jong Sei Kim, Se-Eun Son, Min Bum Kim, Young Sang Cho, Won-Ho Chung
Clin Exp Otorhinolaryngol. 2021;14(3):268-277. doi: 10.21053/ceo.2020.01942.
Reference
-
1. Flint PW, Haughey BH, Lund VJ, Niparko JK, Richardson MA, Robbins KT, et al. Cummings otolaryngology head & neck surgery. 2010. 5th ed. Philadelphia: Mosby.2. Glasscock ME 3rd, Hart MJ, Rosdeutscher JD, Bhansali SA. Traumatic perilymphatic fistula: how long can symptoms persist? A follow-up report. Am J Otol. 1992; 7. 13(4):333–338. PMID: 1415496.3. Hughes GB, Sismanis A, House JW. Is there consensus in perilymph fistula management? Otolaryngol Head Neck Surg. 1990; 2. 102(2):111–117. PMID: 2113234.
Article4. Sim RJ, Jardine AH, Beckenham EJ. Long-term outcome of children undergoing surgery for suspected perilymph fistula. J Laryngol Otol. 2009; 3. 123(3):298–302. PMID: 18577270.
Article5. Goto F, Ogawa K, Kunihiro T, Kurashima K, Kobayashi H, Kanzaki J. Perilymph fistula: 45 case analysis. Auris Nasus Larynx. 2001; 1. 28(1):29–33. PMID: 11137360.6. Hillman TA, Kertesz TR, Hadley K, Shelton C. Reversible peripheral vestibulopathy: the treatment of superior canal dehiscence. Otolaryngol Head Neck Surg. 2006; 3. 134(3):431–436. PMID: 16500440.
Article7. House JW, Morris MS, Kramer SJ, Shasky GL, Coggan BB, Putter JS. Perilymphatic fistula: surgical experience in the United States. Otolaryngol Head Neck Surg. 1991; 7. 105(1):51–61. PMID: 1909008.
Article8. Black FO, Pesznecker S, Norton T, Fowler L, Lilly DJ, Shupert C, et al. Surgical management of perilymphatic fistulas: a Portland experience. Am J Otol. 1992; 5. 13(3):254–262. PMID: 1609855.9. Seltzer S, McCabe BF. Perilymph fistula: the Iowa experience. Laryngoscope. 1986; 1. 96(1):37–49. PMID: 3941579.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Barotraumatic Perilymph Fistula Mimicking Atypical Benign Paroxysmal Positional Vertigo with Sudden Hearing Loss
- Two Cases of Idiopathic Progressive Sensorineural Hearing Loss with Positional Nystagmus in Postpartum Period: Possible Spontaneous Perilymph Fistula?
- A Case of Multiple Perilymph Fistula Induced by Tympanostomy Tube Insertion
- A Case of Intractable Suspected Perilymph Fistula with Severe Depression
- Acute effects of sodium salicylate on concentrations of catecholamine in the perilymph