J Korean Orthop Assoc.
2012 Jun;47(3):216-221. 10.4055/jkoa.2012.47.3.216.
Gossypiboma Mimicking a Soft Tissue Tumor
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Hanyang University, Seoul, Korea. chhchoi@hanyang.ac.kr
- KMID: 2106651
- DOI: http://doi.org/10.4055/jkoa.2012.47.3.216
Abstract
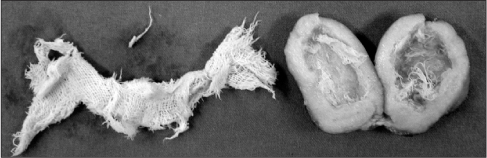
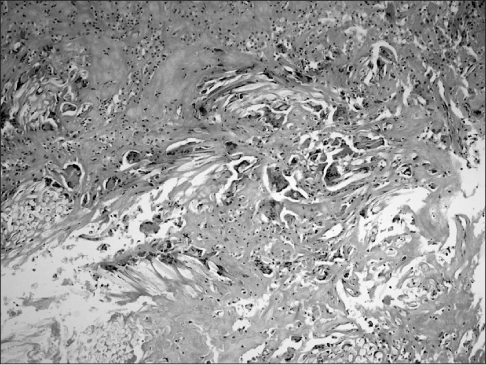
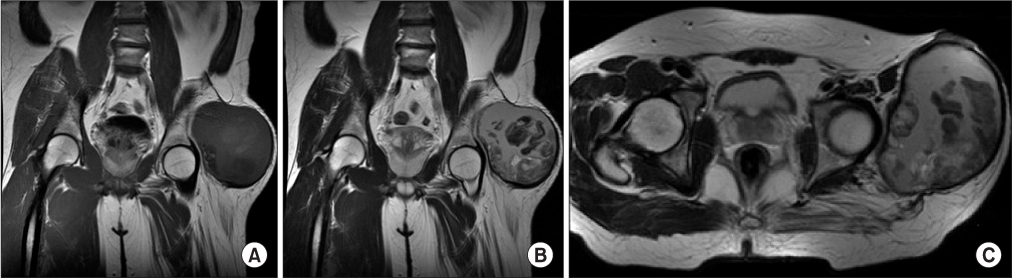
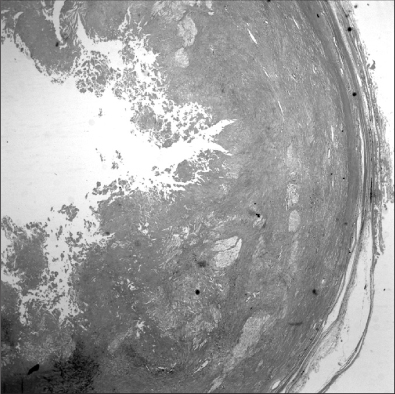
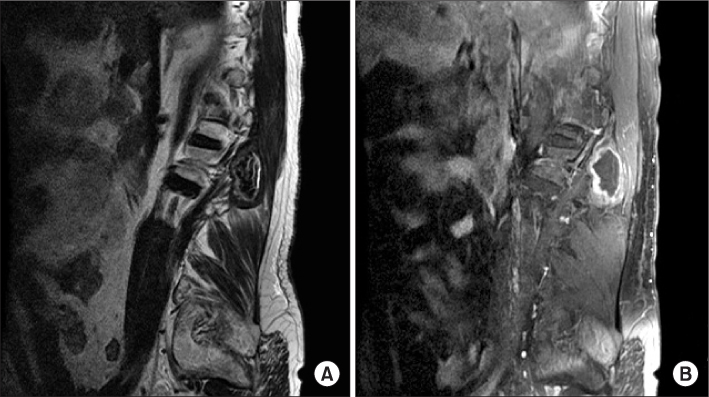
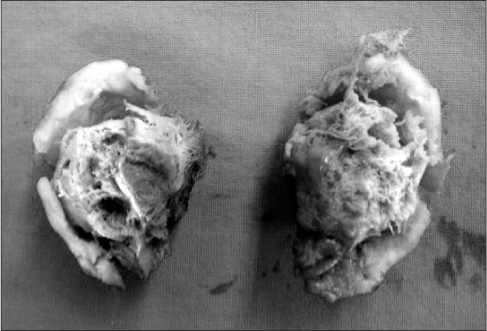
- Paraspinal or extremity foreign-body reactions are a rare disease, which could be caused by foreign bodies to prevent intraoperative bleeding and can result in severe complications or death. However, they are often neglected. We report three cases of paraspinal and parapelvic gossypiboma mimicking a soft tissue tumor on magnetic resonance imaging, which were diagnosed and treated by surgical excision.
Keyword
Figure
Reference
-
1. Park JS, Park DI. Gossypiboma (Textiloma) due to retained surgical gauze. Korean J Gastroenterol. 2006. 48:143–144.2. Rajković Z, Altarac S, Papeš D. An unusual cause of chronic lumbar back pain: retained surgical gauze discovered aft er 40 years. Pain Med. 2010. 11:1777–1779.3. Ramirez LF, Thisted R. Complications and demographic characteristics of patients undergoing lumbar discectomy in community hospitals. Neurosurgery. 1989. 25:226–230.
Article4. Nabors MW, McCrary ME, Clemente RJ, et al. Identification of a retained surgical sponge using magnetic resonance imaging. Neurosurgery. 1986. 18:496–498.
Article5. Matsuki M, Matsuo M, Okada N. Case report: MR findings of a retained surgical sponge. Radiat Med. 1998. 16:65–67.6. Okten AI, Adam M, Gezercan Y. Textiloma: a case of foreign body mimicking a spinal mass. Eur Spine J. 2006. 15:626–629.
Article7. Massie JB, Heller JG, Abitbol JJ, McPherson D, Garfin SR. Postoperative posterior spinal wound infections. Clin Orthop Relat Res. 1992. 284:99–108.
Article8. Marquardt G, Rettig J, Lang J, Seifert V. Retained surgical sponges, a denied neurosurgical reality? Cautionary note. Neurosurg Rev. 2001. 24:41–43.
Article9. Manzella A, Filho PB, Albuquerque E, Farias F, Kaercher J. Imaging of gossypibomas: pictorial review. AJR Am J Roentgenol. 2009. 193:S94–S101.10. Turgut M, Akyüz O, Ozsunar Y, Kacar F. Sponge-induced granuloma ("gauzoma") as a complication of posterior lumbar surgery. Neurol Med Chir (Tokyo). 2005. 45:209–211.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracranial Gossypiboma Mimicking a Recurrent Low Grade Astrocytoma: Case Report
- Gossypiboma of the Thigh: Characteristic MRI Findings. A Case Report
- Various Tumor-Mimicking Lesions in the Musculoskeletal System: Causes and Diagnostic Approach
- Subungual Hypervascular Soft Tissue Chondroma Mimicking a Glomus Tumor: A Case Report
- Gossypiboma of the Neck Mimicking an Isolated Neck Recurrence