J Korean Soc Radiol.
2012 Sep;67(3):149-156. 10.3348/jksr.2012.67.3.149.
Increased Detection Rate of Syringomyelia by Whole Spine Sagittal Magnetic Resonance Images: Based on the Data from Military Conscription of Korean Young Males
- Affiliations
-
- 1Seoul Regional Military Manpower Administration, Seoul, Korea.
- 2Department of Neurosurgery, Inha University Hospital, College of Medicine, Inha University, Incheon, Korea. nsyoon@gmail.com
- 3Department of Radiology, Inha University Hospital, College of Medicine, Inha University, Incheon, Korea.
- KMID: 2097964
- DOI: http://doi.org/10.3348/jksr.2012.67.3.149
Abstract
- PURPOSE
We compared the detection rate of syringomyelia according to the type of magnetic resonance (MR) images among the Korean military conscription.
MATERIALS AND METHODS
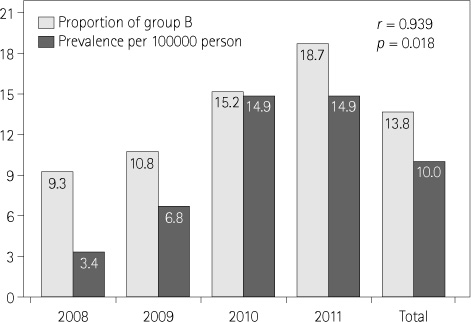
Among the total of 238910 examinees (males aged 18 to 32 years old) from January 2008 to December 2011, the examinees with conventional single lesion MR images (cervical, thoracic, and lumbar) with and without whole spine sagittal T2-weighted MR images (WSST2I) totaled 1206 cases, and syringomyelia was observed in 24 cases. The detection rate of syringomyelia according to the MR protocol (the presence of WSST2I or not) was done through analysis by annually and the clinical characters of syringomyelia was reviewed.
RESULTS
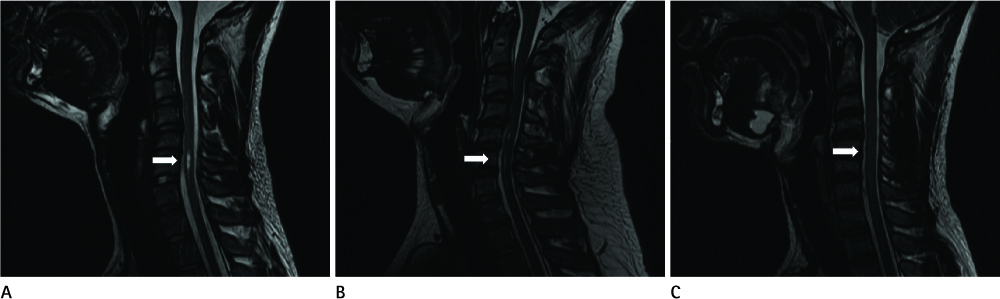
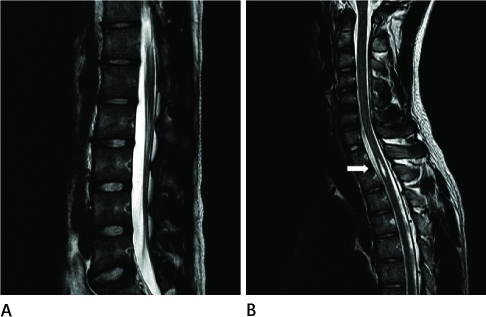
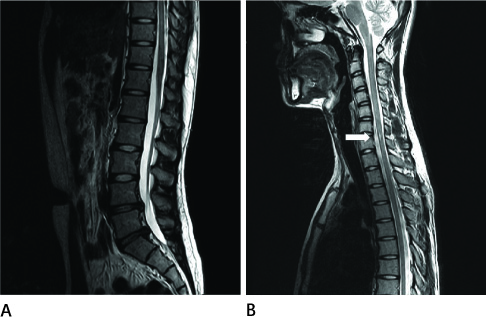
The estimated prevalence of syringomyelia was approximately 10.0 cases per 100000 people. The detection rate was increased annually when the WSST2I proportion was increased (from 3.4 to 14.9 cases per 100000 persons, r = 0.939, p = 0.018). Clinical character of syringomyelia was ambiguous with other spinal diseases. The most affected spinal level was C5 to C7 (83%), and most cases were non-communicating syringomyelia with benign central canal widening (79%).
CONCLUSION
Whole spine sagittal MR image is useful to detect coexisting spinal diseases such as syringomyelia, and most syringomyelia in young males was benign hydromyelia. A whole spine sagittal MR image is recommended to increase the detection of syringomyelia.
MeSH Terms
Figure
Reference
-
1. Barnett HJ, Botterell EH, Jousse AT, Wynn-Jones M. Progressive myelopathy as a sequel to traumatic paraplegia. Brain. 1966. 89:159–174.2. Bastian HC. On a Case of Concussion-Lesion, with extensive secondary degenerations of the Spinal Cord, followed by General Muscular Atrophy. Med Chir Trans. 1867. 50:499–542.1.3. Phillips WA, Hensinger RN, Kling TF Jr. Management of scoliosis due to syringomyelia in childhood and adolescence. J Pediatr Orthop. 1990. 10:351–354.4. Williams B. Pathogenesis of post-traumatic syringomyelia. Br J Neurosurg. 1992. 6:517–520.5. Williams B, Terry AF, Jones F, McSweeney T. Syringomyelia as a sequel to traumatic paraplegia. Paraplegia. 1981. 19:67–80.6. Umbach I, Heilporn A. Review article: post-spinal cord injury syringomyelia. Paraplegia. 1991. 29:219–221.7. Heiss JD, Oldfield EH. Pathophysiology and treatment of syringomyelia. Contemp Neurosurg. 2003. 25:1–8.8. Milhorat TH. Classification of syringomyelia. Neurosurg Focus. 2000. 8:E1.9. Byun MS, Shin JJ, Hwang YS, Park SK. Decompressive surgery in a patient with posttraumatic syringomyelia. J Korean Neurosurg Soc. 2010. 47:228–231.10. Cho KH, Iwasaki Y, Imamura H, Hida K, Abe H. Experimental model of posttraumatic syringomyelia: the role of adhesive arachnoiditis in syrinx formation. J Neurosurg. 1994. 80:133–139.11. Koyanagi I, Iwasaki Y, Hida K, Houkin K. Clinical features and pathomechanisms of syringomyelia associated with spinal arachnoiditis. Surg Neurol. 2005. 63:350–355. discussion 355-356.12. Rossier AB, Foo D, Shillito J, Dyro FM. Posttraumatic cervical syringomyelia. Incidence, clinical presentation, electrophysiological studies, syrinx protein and results of conservative and operative treatment. Brain. 1985. 108(Pt 2):439–461.13. Alexander MA, Bunch WH, Ebbesson SO. Can experimental dorsal rhizotomy produce scoliosis? J Bone Joint Surg Am. 1972. 54:1509–1513.14. Alvisi C, Cerisoli M. Long-term results of the surgical treatment of syringohydromyelia. Acta Neurochir (Wien). 1984. 71:133–140.15. Chuma A, Kitahara H, Minami S, Goto S, Takaso M, Moriya H. Structural scoliosis model in dogs with experimentally induced syringomyelia. Spine (Phila Pa 1976). 1997. 22:589–594. discussion 595.16. Gardner JW, Collis JS. Skeletal anomalies associated with syringomyelia, diastematomyelia, and myelomeningocele. J Bone Joint Surg Am. 1960. 42:1265.17. Gurr KR, Taylor TK, Stobo P. Syringomyelia and scoliosis in childhood and adolescence. J Bone Joint Surg Am. 1988. 70:159.18. Merck manual for healthcare professional. Syrinx [Internet]. c2007. Cited 2007 Jan. Merck Sharp & Dohme Corp;Merck. Available from: http://www.merckmanuals.com/professional.19. Tomlinson RJ Jr, Wolfe MW, Nadall JM, Bennett JT, MacEwen GD. Syringomyelia and developmental scoliosis. J Pediatr Orthop. 1994. 14:580–585.20. Jinkins JR, Sener RN. Idiopathic localized hydromyelia: dilatation of the central canal of the spinal cord of probable congenital origin. J Comput Assist Tomogr. 1999. 23:351–353.21. Moriwaka F, Tashiro K, Tachibana S, Yada K. [Epidemiology of syringomyelia in Japan--the nationwide survey]. Rinsho Shinkeigaku. 1995. 35:1395–1397.22. Schmitz A, Jaeger UE, Koenig R, Kandyba J, Wagner UA, Giesecke J, et al. A new MRI technique for imaging scoliosis in the sagittal plane. Eur Spine J. 2001. 10:114–117.23. Schmitz A, Kandyba J, Koenig R, Jaeger UE, Gieseke J, Schmitt O. A new method of MR total spine imaging for showing the brace effect in scoliosis. J Orthop Sci. 2001. 6:316–319.24. Althoff CE, Appel H, Rudwaleit M, Sieper J, Eshed I, Hamm B, et al. Whole-body MRI as a new screening tool for detecting axial and peripheral manifestations of spondyloarthritis. Ann Rheum Dis. 2007. 66:983–985.25. Green RA, Saifuddin A. Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol. 2004. 33:129–135.26. Kaila R, Malhi AM, Mahmood B, Saifuddin A. The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech. 2007. 20:78–81.27. Ramachandran M, Tsirikos AI, Lee J, Saifuddin A. Whole-spine magnetic resonance imaging in patients with neurofibromatosis type 1 and spinal deformity. J Spinal Disord Tech. 2004. 17:483–491.28. Nakanishi K, Kobayashi M, Nakaguchi K, Kyakuno M, Hashimoto N, Onishi H, et al. Whole-body MRI for detecting metastatic bone tumor: diagnostic value of diffusion-weighted images. Magn Reson Med Sci. 2007. 6:147–155.29. Han IH, Suh SH, Kuh SU, Chin DK, Kim KS. Types and prevalence of coexisting spine lesions on whole spine sagittal MR images in surgical degenerative spinal diseases. Yonsei Med J. 2010. 51:414–420.30. Hanson EH, Mishra RK, Chang DS, Perkins TG, Bonifield DR, Tandy RD, et al. Sagittal whole-spine magnetic resonance imaging in 750 consecutive outpatients: accurate determination of the number of lumbar vertebral bodies. J Neurosurg Spine. 2010. 12:47–55.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Missed Diagnosis of Syrinx
- The Prevalence of Urologic Disease in Young Men Based on a Review of Korean Military Conscription Examination Results
- Prevalence of Lumbar Disc Herniation in Adolescent Males in Seoul, Korea: Prevalence of Adolescent LDH in Seoul, Korea
- Cervical Syringomyelia Associated with Cerebellar Mixed Oligo-Astrocytoma: A Case Report
- Diastematomyelia: A Surgical Case with Long-Term Follow-Up