J Korean Soc Radiol.
2011 Feb;64(2):139-146. 10.3348/jksr.2011.64.2.139.
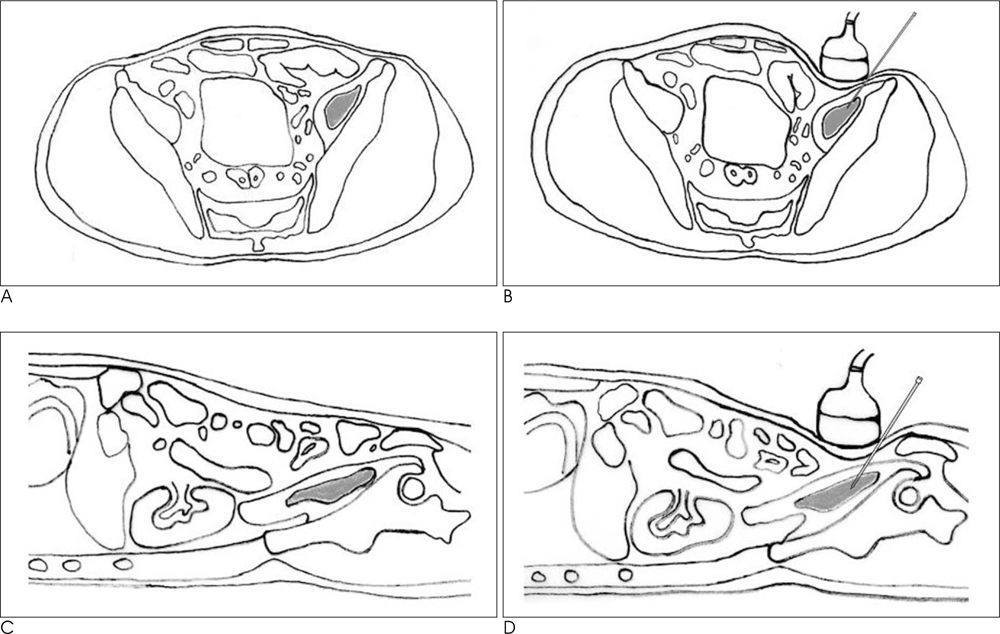
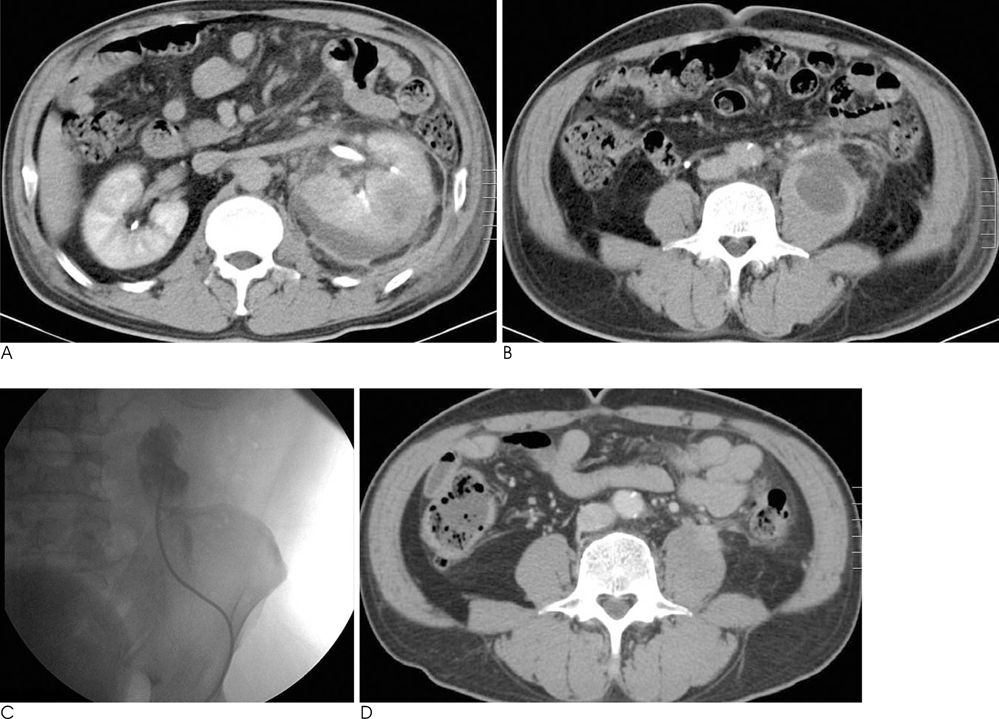
Effectiveness of Fluoroscopic and US - Guided Percutaneous Catheter Drainage for Iliopsoas Abscess through the Anterolateral Transabdominal Approach
- Affiliations
-
- 1Department of Radiology, Gyeongsang National University, College of Medicine, Jinju, Korea. jaro2@hanmail.net
- KMID: 2097929
- DOI: http://doi.org/10.3348/jksr.2011.64.2.139
Abstract
- PURPOSE
We evaluated the effectiveness of performing fluoroscopic and ultrasonography guided percutaneous catheter drainage (PCD) through the anterolateral transabdominal approach for treating iliopsoas abscess.
MATERIALS AND METHODS
From January 2008 to December 2009, fluoroscopic and US-guided PCD through the anterolateral transabdominal approach was performed on sixteen iliopsoas abscesses of fourteen patients (7 males and 7 females; mean age: 63 years; age range: 30-87 years). Six abscesses were on the right side and ten abscesses were on the left side. The location of the abscesses were the psoas muscle (n=7), the iliacus muscle (n=7) and the iliopsoas muscle (n=2). All the procedures were performed under fluoroscopy and US guidance in the angiography room. The clinical findings before and after the procedure, the duration of catheter insertion and the procedure-related complications were evaluated.
RESULTS
15 out of the 16 iliopsoas abscesses were effectively treated. The duration of catheter insertion was 5-27 days (mean: 14.6) days. No patient had significant complications during or after drainage. One patient died of uncontrolled diabetes complications and shock on the 9th day after percutaneous catheter drainage. One recurrence was noted 5 months after removal of the catheter. This patient underwent aspiration and antibiotic treatment for this lesion and the patient improved.
CONCLUSION
Fluoroscopic and US-guided PCD for iliopsoas abscess through the anterolateral transabdominal approach is an effective and safe procedure.
MeSH Terms
Figure
Reference
-
1. Dinc H, Onder C, Turhan AU, Sari A, Aydin A, Yulug G, et al. Percutaneous drainage of tuberculous and nontuberculous psoas abscesses. Eur J Radiol. 1996; 23:130–134.2. Muller PR, Ferrucci JT Jr, Wittenberg J, Simeone JF, Butch RJ. Iliopsoas abscess : treatment by CT-guided percutaneous catheter drainage. AJR Am J Roentgenol. 1984; 142:359–362.3. Gupta S, Suri S, Gulati M, Singh P. Ilio-psoas abscess. Percutaneous drainage under image guidance. Clin Radiol. 1997; 52:704–707.4. Pombo F, Martin-Egana R, Cela A, Diaz JL, Linares-Mondejar P, Freire M. Percutaneous catheter drainage of tuberculous psoas abscesses. Acta Radiol. 1993; 155:366–368.5. Cantasdemir M, Kara B, Cebi D, Selcuk ND, Numan F. Computed tomography-guided percutaneous catheter drainage of primary and seconddary iliopsoas abscess. Clin Radiol. 2003; 58:811–815.6. Gupta S, Nguyen HL, Morello FA Jr., Ahrar K, Wallace MJ, Madoff DC, et al. Various approaches for CT-guided percutaneous biopsy of deep pelvic lesions: anatomic and technical considerations. Radiographics. 2004; 24:175–189.7. Maher MM, Gervais DA, Kalra MK, Lucey B, Sahani DV, Arellano R, et al. The inaccessible or undrainable abscess: how to drain it. Radiographics. 2004; 24:717–735.8. Tanomkiat W, Buranapanitkit B. Percutaneous drainage of large tuberculous iliopsoas abscess via a subinguinal approach: a report of two casces. J Orthop Sci. 2004; 9:157–161.9. Ralls PW, Boswell W, Henderson R, Rogers W, Boger D, Halls J. CT of inflammatory disease of the psoas muscle. AJR Am J Roentgenol. 1980; 134:767–770.10. Sheikh M, Al-Ali AA, Al-Sumait B, Behbehani A. CT-guided percutaneous drainage of tuberculous and non-tuberculous deep pelvic abscesses. Med Princ Pract. 2000; 9:52–58.11. Desandre AR, Cottone FJ, Evers ML. Iliopsoas abscess: etiology, diagnosis and treatment. Am Surg. 1995; 61:1087–1091.12. Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: case report and review of the literature. J Urol. 1992; 147:1624–1626.13. Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: worldwide variations in etiology. World J Surg. 1986; 10:834–843.14. Harris LF, Sparks JE. Retroperitoneal abscess: case report and review of the literature. Dig Dis Sci. 1980; 25:392–394.15. Santaella RO, Fishman EK, Lipsett PA. Primary vs secondary iliopsoas abscess: presentation, microbiology, and treatment. Arch Surg. 1995; 130:1309–1313.16. 2005. 68:205–210.17. Lobo DN, Dunn WK, Iftikhar SY, Scholefield JH. Psoas abscess complicating colonic disease: imaging and therapy. Ann R Coll Surg Engl. 1998; 80:405–409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Drainage of Postoperative Pelvic Abscess: Fluoroscopic and US-Guided Transgluteal Approach
- Effectiveness of Percutaneous Catheter Drainage for Tuberculous Iliopsoas Abscess associated with Tuberculous Spondylitis
- Percutaneous catheter drainage of intraabdominal abscess
- Transrectal Drainage of Deep Pelvic Abscesses
- Percutaneous Catheter Drainage of Intrapulmonary Fluid Collection