J Korean Soc Radiol.
2010 Nov;63(5):425-430. 10.3348/jksr.2010.63.5.425.
Usefulness of Interventional Treatment for Dysfunctional Hemodialysis Shunts of the Upper Arm by Means of the Retrograde Transradial Approach
- Affiliations
-
- 1Department of Radiology, Gyeongsang National University Hospital, Korea.
- 2Department of Radiology, Institute of Health Science, Gyeongsang National University Hospital, Korea. tbshinkr@yahoo.co.kr
- 3Department of Nephology, Gyeongsang National University Hospital, Korea.
- 4Department of Chest Surgery, Gyeongsang National University Hospital, Korea.
- 5Department of Radiology, Masan Samsung Hospital, Sungkyunkwan University, Korea.
- 6Department of Radiology, Kosin University Hospital, Korea.
- KMID: 2097912
- DOI: http://doi.org/10.3348/jksr.2010.63.5.425
Abstract
- PURPOSE
This study was designed to evaluate the technical feasibility and clinical outcome of endovascular intervention using the retrograde transradial approach to treat dysfunctional hemodialysis shunts of the upper arms.
MATERIALS AND METHODS
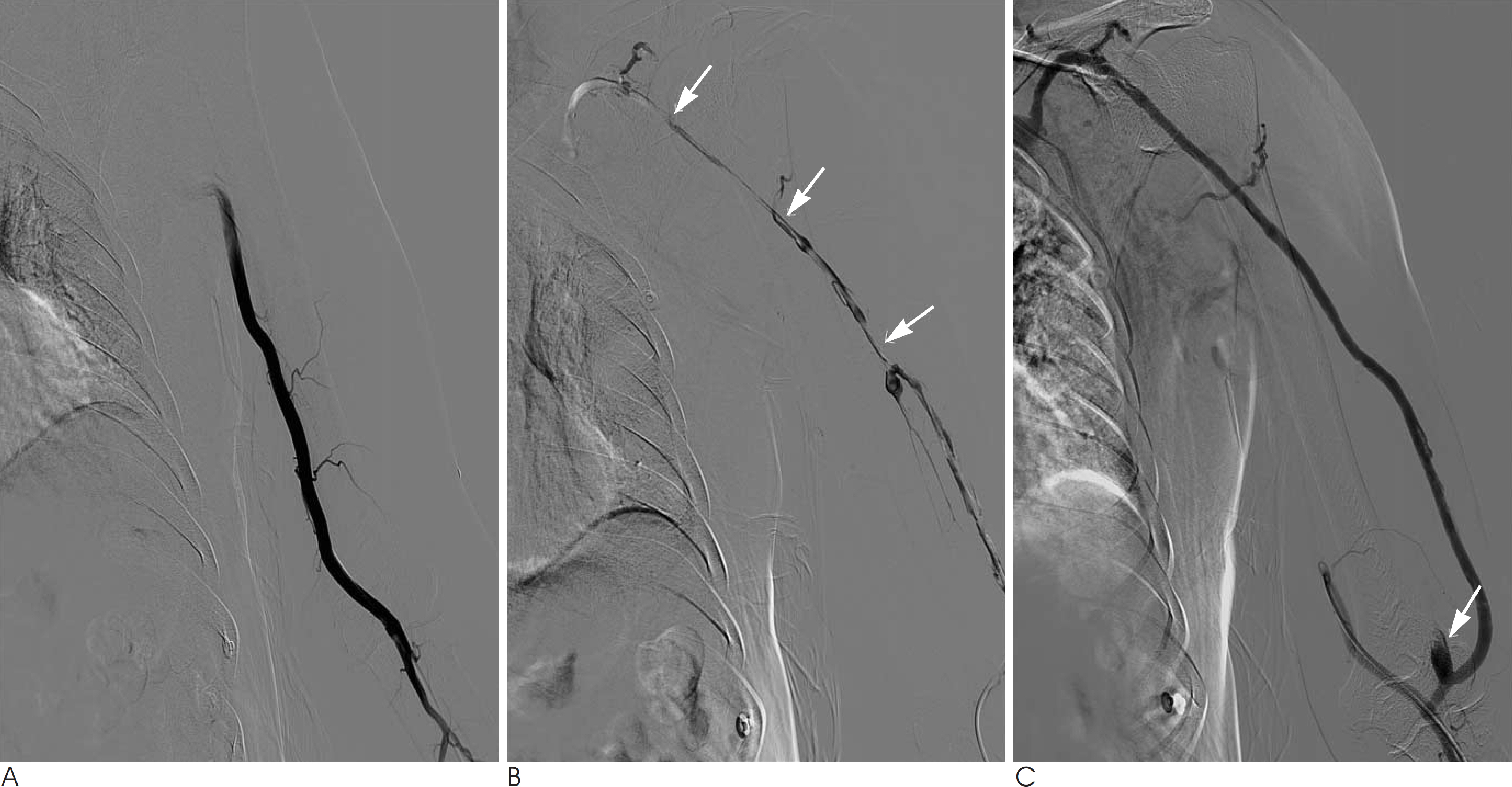
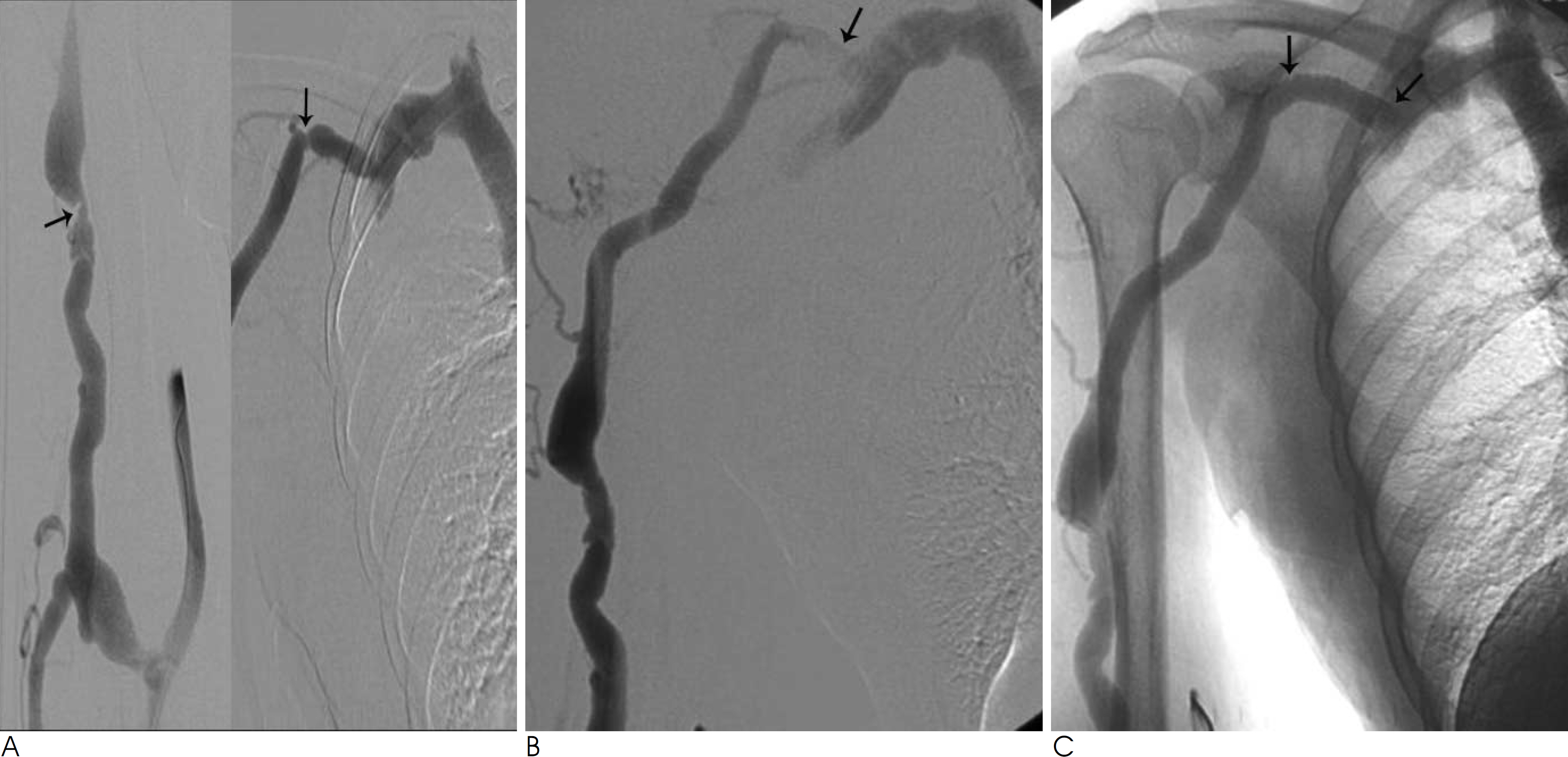
During the last 3 years, sixteen procedures were performed by the transradial approach in 13 patients with dysfunctional hemodialysis shunts of the upper arms. The radial artery was accessedwith the use of 20-gauge needle and a 6-Fr sheath. Angiography was performed using a 5-Fr catheter placed in the brachial artery, and then the interventional procedure was performed. The technical and clinical success rates, complications and patency rates were evaluated.
RESULTS
Fistulography and percutaneous transluminal angioplasty via the transradial approach were performed in 16 cases of the 13 patients. Fistulography demonstrated stenosis in 7 cases and occlusions in 9 cases. Lesion multiplicity was identified in 9 out of 16 cases. Balloon angioplasty was performed in all cases and a stent was placed to overcome restenosis or to treat venous rupture in two cases. The technical success rate of balloon angioplasty was 87.5% (14/16) and the technical success rate with including stent insertion was 100%(16/16). The clinical success rate was 93.8%. There was one procedural-related complication. The primary patency rates at 6 and 12 months were 84.6% and 74%, respectively.
CONCLUSION
The transradial approach seems to be technically feasible and effective for the management of insufficient hemodialysis shunts of the upper arms.
MeSH Terms
Figure
Reference
-
1. Gallego Beuter JJ, Hernandez Lezana A, Herrero Calvo J, Moreno Carriles R. Early detection and treatment of hemodialysis access dysfunction. Cardiovasc Intervent Radiol. 2000; 23:40–46.
Article2. Tessitore N, Mansueto G, Bedogna V, Lipari G, Poli A, Gammaro L, et al. A prospective controlled trial on effect of percutaneous transluminal angioplasty on functioning arteriovenous fistulae sur-vival. J Am Soc Nephrol. 2003; 14:1623–1627.
Article3. Zaleski GX, Funaki B, Kenney S, Lorenz JM, Garofalo R. Angioplasty and bolus urokinase infusion for the restoration of function in thrombosed Brescia-Cimino fistula. J Vasc Interv Radiol. 1999; 10:129–136.4. Miyayama S, Matsui O, Taki K, Minami T, Shinmura R, Ito C, et al. Occluded Brescia-Cimino hemodialysis fistulas: endovascular treatment with both brachial arterial and venous access using pull-through technique. Cardiovasc Intervent Radiol. 2005; 28:806–812.5. Rajan DK, Clark TW, Vatel NK, Stavropoulos SW, Simons ME. Prevalence and treatment of cephalic arch stenosis in dysfunctional autogenous hemodialysis fistulas. J Vasc Interv Radiol. 2003; 14:567–573.
Article6. Manninen HI, Kaukanen ET, Ikaheimo R, Karhapaa P, Lahtinen T, Matsi P, et al. Brachial arterial access: endovascular treatment of failing Brescia-Cimino hemodialysis fistulas–initial success and long term results. Radiology. 2001; 218:711–718.7. Jeon UB, Kim CW, Chung SW. Percutaneous treatment of thrombosed prosthetic brachial-basilic access by the transradial approach. J Vasc Surg. 2009; 49:1057–1059.
Article8. Held PJ, Port FK, Wolfe RA, Stannard DC, Carroll CE, Daugirdas JT, et al. The dose of hemodialysis and patient mortality. Kidney Int. 1996; 50:550–556.
Article9. Wang HJ, Yang YF. Percutaneous treatment of dysfunctional Brescia-Cimino fistulae through a radial arterial approach. Am J Kidney Dis. 2006; 48:652–658.
Article10. Gmelin E, Winterhoff R, Rinast E. Insufficient hemodialysis access fistulas. Late results of treatment with percutaneous balloon angioplasty. Radiology. 1989; 171:657–660.
Article11. Turmel-Rodrigues L, Mouton A, Birmele B, Billaux L, Ammar N, Grezard O, et al. Salvage of immature forearm fistulas for hemodialysis by interventional radiology. Nephrol Dial Transplant. 2001; 16:2365–2371.12. Liang HL, Pan HB, Chung HM, Ger LP, Fang HC, Wu TH, et al. Restoration of thrombosed Brescia-Cimino dialysis fistulas by using percutaneous transluminal angioplasty. Radiology. 2002; 223:339–344.
Article13. Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989; 16:3–7.
Article14. Agostoni P, Biondi-Zoccai GG, de Benedictis ML, Rigattieri S, Turri M, Anselmi M, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures: systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004; 44:349–356.
Article15. Scheinert D, Braunlich S, Nonnast-Daniel B, Schroeder M, Schmidt A, Biamino G, et al. Transradial approach for renal artery stenting. Catheter Cardiovasc Interv. 2001; 54:442–447.
Article16. Fessler RD, Wakhloo AK, Lanzino G, Guterman LR, Hopkins LN. Transradial approach for vertebral artery stenting: technical case report. Neurosurgery. 2000; 46:1542–1547.
Article17. Raghu C, Louvard Y. Transradial approach for percutaneous transluminal angioplasty and stenting in the treatment of chronic mesenteric ischemia. Catheter Cardiovasc Interv. 2004; 61:450–454.
Article18. Kawarada O, Yokoi Y, Nakata S, Morioka N, Takemoto K. Transradial intervention for native fistula failure. Catheter Cardiovasc Interv. 2006; 68:513–520.
Article19. Louvard Y, Lefe`vre T. Loops and transradial approach in coronary diagnosis and intervention. Catheter Cardiovasc Interv. 2000; 51:250–252.
Article20. Sakai H, Ikeda S, Harada T, Yonashiro S, Ozumi K, Ohe H, et al. Limitations of successive transradial approach in the same arm: the japanese experience. Catheter Cardiovasc Interv. 2001; 54:204–208.
Article21. Kanterman RY, Vesely TM, Pilgram TK, Guy BW, Windus DW, Picus D. Dialysis access grafts: anatomic location of venous stenosis and results of angioplasty. Radiology. 1995; 195:135–139.
Article22. Turmel-Rodrigues L, Pengolan J, Blanchier D, Abaza M, Birmele B, Haillot O, et al. Insufficient dialysis shunts: improved longterm patency rates with close hemodynamic monitoring, repeated percutaneous balloon angioplasty, and stent placement. Radiology. 1993; 187:273–278.
Article23. Beathard GA. Percutaneous transvenous angioplasty in the treatment of vascular access stenosis. Kidney Int. 1992; 42:1390–1397.
Article24. Safa AA, Valji K, Roberts AC, Ziegler TW, Hye RJ, Oglevie SB. Detection and treatment of dysfunctional hemodialysis access grafts: effect of a surveillance program on graft pateny and the inci-dence of thrombosis. Radiology. 1996; 199:653–657.25. Beathard GA, Litchfield T. Physician Operator Forum of RMS Lifeline, INC. Effectiveness and safety of dialysis vascular access procedures performed by interventional nephrologists. Kidney Int. 2004; 66:1622–1632.26. Turmel-rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, et al. Treatment of stenosis and thrombosis in hemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000; 15:2029–2036.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Transradial Approach for Coronary Angiography
- Transradial Approach for Thoracolumbar Spinal Angiography and Tumor Embolization: Feasibility and Technical Considerations
- Endovascular Treatment of Cavernous Sinus Dural Arteriovenous Fistula via Radial Artery and Median Cubital Vein
- A Case of Transradial Approach to Carotid Artery Angioplasty and Stenting in Left Internal Carotid Stenosis
- RE: Endovascular Treatment of Congenital Intrahepatic Portosystemic Shunts with Amplatzer Plugs