Neurointervention.
2022 Jul;17(2):100-105. 10.5469/neuroint.2022.00010.
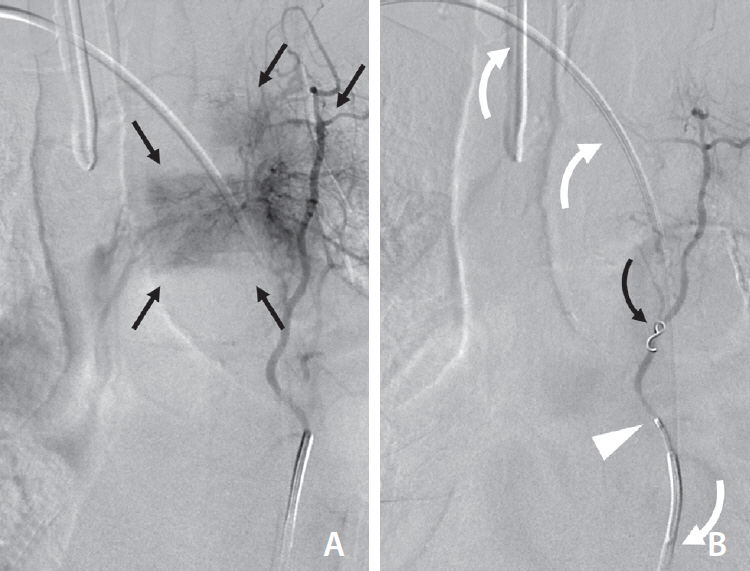
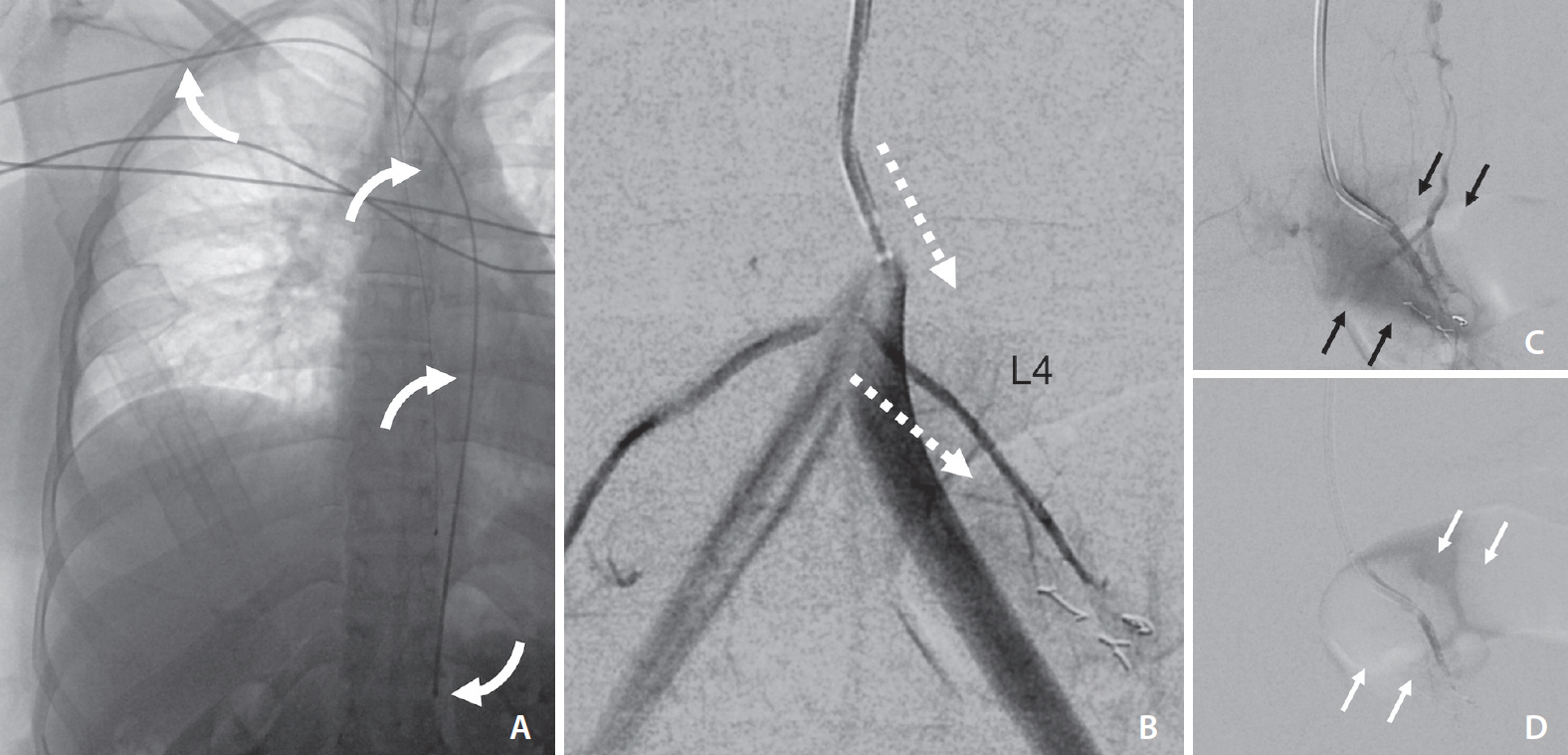
Transradial Approach for Thoracolumbar Spinal Angiography and Tumor Embolization: Feasibility and Technical Considerations
- Affiliations
-
- 1Department of Neurointerventional Radiology, University of California San Francisco, San Francisco, CA, USA
- 2Department of Neurological Surgery, University of California San Francisco, San Francisco, CA, USA
- KMID: 2531565
- DOI: http://doi.org/10.5469/neuroint.2022.00010
Abstract
- The transradial approach (TRA) is an effective and safe alternative to transfemoral access for diagnostic neuroangiography and craniocervical interventions. While the technical aspects of supraclavicular intervention are well-described, there are little data on the TRA for thoracolumbar angiography and intervention. The authors describe the feasibility of the TRA for preoperative thoracic tumor embolization, emphasizing technique, device selection, navigation, and catheterization of thoracolumbar segmental arteries. This approach extends the benefits of TRA to spinal interventional neuroradiology.
Keyword
Figure
Reference
-
1. Wilson MA, Cooke DL, Ghodke B, Mirza SK. Retrospective analysis of preoperative embolization of spinal tumors. AJNR Am J Neuroradiol. 2010; 31:656–660.
Article2. Prabhu VC, Bilsky MH, Jambhekar K, Panageas KS, Boland PJ, Lis E, et al. Results of preoperative embolization for metastatic spinal neoplasms. Neurosurg. 2003; 98(2 Suppl):156–164.
Article3. Gellad FE, Sadato N, Numaguchi Y, Levine AM. Vascular metastatic lesions of the spine: preoperative embolization. Radiology. 1990; 176:683–686.
Article4. Griessenauer CJ, Salem M, Hendrix P, Foreman PM, Ogilvy CS, Thomas AJ. Preoperative embolization of spinal tumors: a systematic review and meta-analysis. World Neurosurg. 2016; 87:362–371.
Article5. Gailloud P. Introduction to diagnostic and therapeutic spinal angiography. Neuroimaging Clin N Am. 2019; 29:595–614.
Article6. Narsinh KH, Mirza MH, Duvvuri M, Caton MT Jr, Baker A, Winkler EA, et al. Radial artery access anatomy: considerations for neuroendovascular procedures. J Neurointerv Surg. 2021; 13:1139–1144.
Article7. Narsinh KH, Mirza MH, Caton MT Jr, Baker A, Winkler E, Higashida RT, et al. Radial artery access for neuroendovascular procedures: safety review and complications. J Neurointerv Surg. 2021; 13:1132–1138.
Article8. Haynes J, Nossek E, Shapiro M, Chancellor B, Frempong-Boadu A, Peschillo S, et al. Radial arterial access for thoracic intraoperative spinal angiography in the prone position. World Neurosurg. 2020; 137:e358–e365.
Article9. Kühn AL, de Macedo Rodrigues K, Singh J, Massari F, Puri AS. Distal radial access in the anatomical snuffbox for neurointerventions: a feasibility, safety, and proof-of-concept study. J Neurointerv Surg. 2020; 12:798–801.
Article10. Orru E, Tsang COA, Klostranec JM, Pereira VM. Republished: transradial approach in the treatment of a sacral dural arteriovenous fistula: a technical note. J Neurointerv Surg. 2019; 11:e4.
Article11. Knox JA, Alexander MD, McCoy DB, Murph DC, Hinckley PJ, Ch’ang JC, et al. Impact of aortic arch anatomy on technical performance and clinical outcomes in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 2020; 41:268–273.
Article12. Luo N, Qi W, Tong W, Meng B, Feng W, Zhou X, et al. The effect of vascular morphology on selective left vertebral artery catheterization in right-sided radial artery cerebral angiography. Ann Vasc Surg. 2019; 56:62–72.
Article13. Hacein-Bey L, Konstas AA, Pile-Spellman J. Natural history, current concepts, classification, factors impacting endovascular therapy, and pathophysiology of cerebral and spinal dural arteriovenous fistulas. Clin Neurol Neurosurg. 2014; 121:64–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Feasibility and Problems in Transradial Coronary Angiography and Intervention
- The Safety and Feasibility of Transradial Coronary Angiography Over 70-Year-Old Patients
- Percutaneous Transradial Approach for Coronary Angiography
- Is Transradial Cerebral Angiography Feasible and Safe? A Single Center's Experience
- A Case of Transradial Approach to Carotid Artery Angioplasty and Stenting in Left Internal Carotid Stenosis