Korean Circ J.
2012 Jul;42(7):449-457. 10.4070/kcj.2012.42.7.449.
The Independent Relationship of Systemic Inflammation With Fragmented QRS Complexes in Patients With Acute Coronary Syndromes
- Affiliations
-
- 1Rize Education and Research Hospital, Department of Cardiology, Rize, Turkey. sinanaltan@gmail.com
- 2Rize University Medical Faculty, Department of Cardiology, Rize, Turkey.
- 3Mehmet Akif Ersoy Education and Research Hospital, Department of Cardiology, Istanbul, Turkey.
- 4Ordu State Hospital, Department of Cardiology, Ordu, Turkey.
- 5Artvin State Hospital, Department of Cardiology, Artvin, Turkey.
- KMID: 2094116
- DOI: http://doi.org/10.4070/kcj.2012.42.7.449
Abstract
- BACKGROUND AND OBJECTIVES
QRS complex fragmentations are frequently seen on routine electrocardiograms with narrow or wide QRS complex. Fragmented QRS complex (fQRS) is associated with increased morbidity and mortality, sudden cardiac death and recurrent cardiovascular events. In this study, we aimed to interrogate the relationship of systemic inflammation with the presence of fQRS in patients with acute coronary syndromes (ACS).
SUBJECTS AND METHODS
Two-hundred and twenty eligible patients with ACS that underwent coronary angiography were enrolled consecutively in this study. Patients with significant organic valve disease and those with any QRS morphology that had a QRS duration > or =120 ms as well as patients with permanent pacemakers were excluded from this study.
RESULTS
Patients with fQRS were of a higher age (p=0.02), had increased C-reactive protein (CRP) levels (p<0.001), prolonged QRS time (p<0.001), extent of coronary artery disease (CAD) (p<0.001), creatine kinase-MB (CK-MB) levels (p=0.006) and Q wave on admission electrocardiography (p<0.001) in comparison to patients with non-fragmented QRS. When we performed multiple logistic regression analysis, fQRS was found to be related to increased CRP levels {odds ratio (OR): 1.2, 95% confidence interval (CI): 1.045-1.316, p=0.007}, QRS duration (OR: 1.1, 95% CI: 1.033-1.098, p<0.001), extent of CAD (OR: 1.5, 95% CI: 1.023-2.144, p=0.037), Q wave (OR: 2.2, 95% CI: 1.084-4.598, p=0.03) and CK-MB levels (OR: 1.0, 95% CI: 1.001-1.037, p=0.04) independently.
CONCLUSION
In our study, we found that fQRS was independently related to increased CRP. Fragmented QRS that may result as an end effect of inflammation at cellular level can represent increased cardiac risk by different causative mechanisms in patients with ACS.
Keyword
MeSH Terms
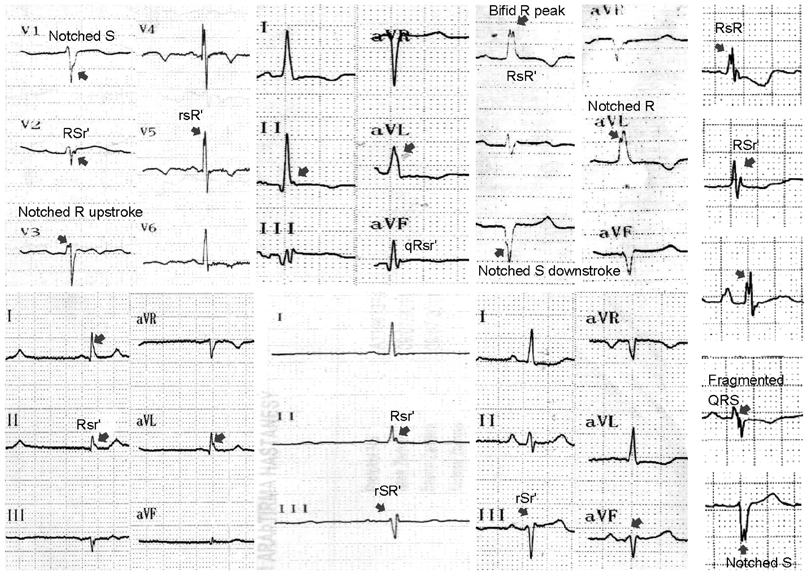
Figure
Reference
-
1. Das MK, Suradi H, Maskoun W, et al. Fragmented wide QRS on a 12-lead ECG: a sign of myocardial scar and poor prognosis. Circ Arrhythm Electrophysiol. 2008. 1:258–268.2. Das MK, Michael MA, Suradi H, et al. Usefulness of fragmented QRS on a 12-lead electrocardiogram in acute coronary syndrome for predicting mortality. Am J Cardiol. 2009. 104:1631–1637.3. Korhonen P, Husa T, Konttila T, et al. Fragmented QRS in prediction of cardiac deaths and heart failure hospitalizations after myocardial infarction. Ann Noninvasive Electrocardiol. 2010. 15:130–137.4. Das MK, Saha C, El Masry H, et al. Fragmented QRS on a 12-lead ECG: a predictor of mortality and cardiac events in patients with coronary artery disease. Heart Rhythm. 2007. 4:1385–1392.5. Pietrasik G, Goldenberg I, Zdzienicka J, Moss AJ, Zareba W. Prognostic significance of fragmented QRS complex for predicting the risk of recurrent cardiac events in patients with Q-wave myocardial infarction. Am J Cardiol. 2007. 100:583–586.6. Das MK, Khan B, Jacob S, Kumar A, Mahenthiran J. Significance of a fragmented QRS complex versus a Q wave in patients with coronary artery disease. Circulation. 2006. 113:2495–2501.7. Das MK, Zipes DP. Fragmented QRS: a predictor of mortality and sudden cardiac death. Heart Rhythm. 2009. 6:3 Suppl. S8–S14.8. Cheema A, Khalid A, Wimmer A, et al. Fragmented QRS and mortality risk in patients with left ventricular dysfunction. Circ Arrhythm Electrophysiol. 2010. 3:339–344.9. Das MK, El Masry H. Fragmented QRS and other depolarization abnormalities as a predictor of mortality and sudden cardiac death. Curr Opin Cardiol. 2010. 25:59–64.10. Das MK, Maskoun W, Shen C, et al. Fragmented QRS on twelve-lead electrocardiogram predicts arrhythmic events in patients with ischemic and nonischemic cardiomyopathy. Heart Rhythm. 2010. 7:74–80.11. Gardner PI, Ursell PC, Fenoglio JJ Jr, Wit AL. Electrophysiologic and anatomic basis for fractionated electrograms recorded from healed myocardial infarcts. Circulation. 1985. 72:596–611.12. Chatterjee S, Changawala N. Fragmented QRS complex: a novel marker of cardiovascular disease. Clin Cardiol. 2010. 33:68–71.13. Eisen A, Arnson Y, Dovrish Z, Hadary R, Amital H. Arrhythmias and conduction defects in rheumatological diseases: a comprehensive review. Semin Arthritis Rheum. 2009. 39:145–156.14. Kadi H, Inanir A, Habiboglu A, et al. Frequency of fragmented QRS on ECG is increased in patients with rheumatoid arthritis without cardiovascular disease: a pilot study. Mod Rheumatol. 2012. 22:238–242.15. Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation. 2007. 116:2634–2653.16. Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients with Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007. 116:e148–e304.17. Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983. 51:606.18. Flowers NC, Horan LG, Thomas JR, Tolleson WJ. The anatomic basis for high-frequency components in the electrocardiogram. Circulation. 1969. 39:531–539.19. Lesh MD, Spear JF, Simson MB. A computer model of the electrogram: what causes fractionation? J Electrocardiol. 1988. 21:Suppl. S69–S73.20. Friedman PL, Fenoglio JJ, Wit AL. Time course for reversal of electrophysiological and ultrastructural abnormalities in subendocardial Purkinje fibers surviving extensive myocardial infarction in dogs. Circ Res. 1975. 36:127–144.21. Wiener I, Mindich B, Pitchon R. Fragmented endocardial electrical activity in patients with ventricular tachycardia: a new guide to surgical therapy. Am Heart J. 1984. 107:86–90.22. Basaran Y, Tigen K, Karaahmet T, et al. Fragmented QRS complexes are associated with cardiac fibrosis and significant intraventricular systolic dyssynchrony in nonischemic dilated cardiomyopathy patients with a narrow QRS interval. Echocardiography. 2011. 28:62–68.23. Calore C, Cacciavillani L, Boffa GM, et al. Contrast-enhanced cardiovascular magnetic resonance in primary and ischemic dilated cardiomyopathy. J Cardiovasc Med (Hagerstown). 2007. 8:821–829.24. Reddy CV, Cheriparambill K, Saul B, et al. Fragmented left sided QRS in absence of bundle branch block: sign of left ventricular aneurysm. Ann Noninvasive Electrocardiol. 2006. 11:132–138.25. Mahenthiran J, Khan BR, Sawada SG, Das MK. Fragmented QRS complexes not typical of a bundle branch block: a marker of greater myocardial perfusion tomography abnormalities in coronary artery disease. J Nucl Cardiol. 2007. 14:347–353.26. Weinberg SL, Reynolds RW, Rosenman RH, Katz LN. Electrocardiographic changes associated with patchy myocardial fibrosis in the absence of confluent myocardial infarction; an anatomic correlative study. Am Heart J. 1950. 40:745–759.27. Varriale P, Chryssos BE. The RSR' complex not related to right bundle branch block: diagnostic value as a sign of myocardial infarction scar. Am Heart J. 1992. 123:369–376.28. Bursi F, Weston SA, Killian JM, Gabriel SE, Jacobsen SJ, Roger VL. C-reactive protein and heart failure after myocardial infarction in the community. Am J Med. 2007. 120:616–622.29. Zhang R, Zhang YY, Huang XR, et al. C-reactive protein promotes cardiac fibrosis and inflammation in angiotensin II-induced hypertensive cardiac disease. Hypertension. 2010. 55:953–960.30. Kazumi T, Kawaguchi A, Hirano T, Yoshino G. C-reactive protein in young, apparently healthy men: associations with serum leptin, QTc interval, and high-density lipoprotein-cholesterol. Metabolism. 2003. 52:1113–1116.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Presence of Fragmented QRS on 12-Lead Electrocardiography in Patients with Coronary Artery Ectasia
- Absence and Resolution of Fragmented QRS Predict Reversible Myocardial Ischemia With Higher Probability of ST Segment Resolution in Patients With ST Segment Elevation Myocardial Infarction
- Fragmented QRS and abnormal creatine kinase-MB are predictors of coronary artery disease in patients with angina and normal electrocardiographys
- Retrograde Conduction in Complete Heart Block
- Significance of QRS Scoring System in the Acute Myocardial Infarction