Korean Circ J.
2010 Mar;40(3):131-136. 10.4070/kcj.2010.40.3.131.
Pulmonary Hypertension in Preterm Infants With Bronchopulmonary Dysplasia
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, Korea. eunjbaek@snu.ac.kr
- KMID: 2094073
- DOI: http://doi.org/10.4070/kcj.2010.40.3.131
Abstract
- BACKGROUND AND OBJECTIVES
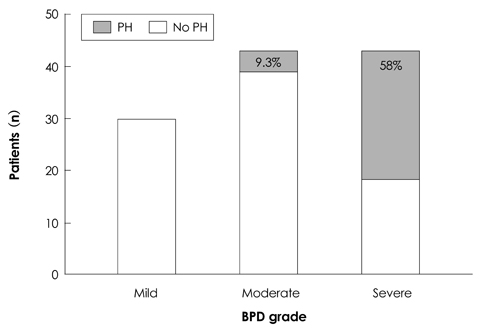
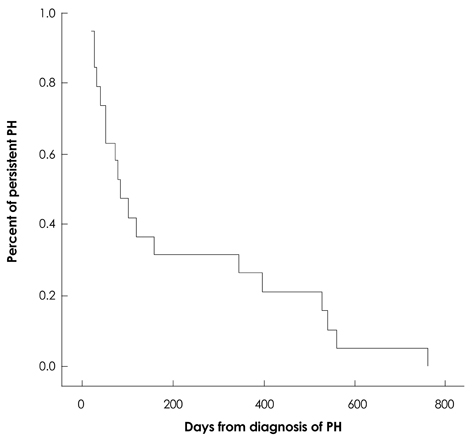
With the increasing survival of preterm infants, pulmonary hypertension (PH) related to bronchopulmonary dysplasia (BPD) has become an important complication. The aim of this study was to investigate the characteristics and outcome of PH in preterm infants with BPD and to identify the risk factors for PH. SUBJECTS AND METHODS: We reviewed the records of 116 preterm infants with BPD cared for at a single tertiary center between 2004 and 2008. RESULTS: Twenty-nine (25%) infants had PH >2 months after birth. PH occurred initially at a median age of 65 days (range, 7-232 days). Severe BPD, a birth weight <800 g, long-term ventilator care and oxygen supplementation, a high ventilator setting, infection, and a patent ductus arteriosus (PDA) were related to PH based on univariate analysis (p<0.05). The infants who had longer oxygen supplementation were significantly more likely to have PH (odds ratio, 18.5; 95% confidence interval, 4.1-84.6; p<0.001). PH was improved in 76% of infants after a median of 85 days (range, 20-765 days). Four infants (14%) died. The death of 3 infants was attributed to PH. CONCLUSION: BPD was frequently complicated by PH. Although PH resolved in the majority of infants, PH in preterm infants with BPD can be fatal. Regular screening for PH and adequate management are required.
MeSH Terms
Figure
Cited by 1 articles
-
Pathophysiology and Risk Factors of Pulmonary Hypertension in Infants with Bronchopulmonary Dysplasia
Do-Hyun Kim
Korean J Perinatol. 2014;25(1):1-8. doi: 10.14734/kjp.2014.25.1.1.
Reference
-
1. Stenmark KR, Abman SH. Lung vascular development: implications for the pathogenesis of bronchopulmonary dysplasia. Annu Rev Physiol. 2005. 67:623–661.2. Abman SH, Accurso FJ, Bowman CM. Unsuspected cardiopulmonary abnormalities complicating bronchopulmonary dysplasia. Arch Dis Child. 1984. 59:966–970.3. Gill AB, Weindling AM. Pulmonary artery pressure changes in the very low birthweight infant developing chronic lung disease. Arch Dis Child. 1993. 68(3 Spec No):303–307.4. Goodman G, Perkin RM, Anas NG, Sperling DR, Hicks DA, Rowen M. Pulmonary hypertension in infants with bronchopulmonary dysplasia. J Pediatr. 1988. 112:67–72.5. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001. 163:1723–1729.6. Khemani E, McElhinney DB, Rhein L, et al. Pulmonary artery hypertension in formerly premature infants with bronchopulmonary dysplasia: clinical features and outcomes in the surfactant era. Pediatrics. 2007. 120:1260–1269.7. Fouron JC, Le Guennec JC, Villemant D, Perreault G, Davignon A. Value of echocardiography in assessing the outcome of bronchopulmonary dysplasia of the newborn. Pediatrics. 1980. 65:529–535.8. Bancalari E, Claure N. Definitions and diagnostic criteria for bronchopulmonary dysplasia. Semin Perinatol. 2006. 30:164–170.9. Subhedar NV. Recent advances in diagnosis and management of pulmonary hypertension in chronic lung disease. Acta Paediatr Suppl. 2004. 93:29–32.10. Abman SH, Wolfe RR, Accurso FJ, Koops BL, Bowman CM, Wiggins JW Jr. Pulmonary vascular response to oxygen in infants with severe bronchopulmonary dysplasia. Pediatrics. 1985. 75:80–84.11. Donti A, Formigari R, Ragni L, Manes A, Galie N, Picchio FM. Pulmonary arterial hypertension in the pediatric age. J Cardiovasc Med (Hagerstown). 2007. 8:72–77.12. Mourani PM, Ivy DD, Gao D, Abman SH. Pulmonary vascular effects of inhaled nitric oxide and oxygen tension in bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2004. 170:1006–1013.13. Berman W Jr, Yabek SM, Dillon T, Burstein R, Corlew S. Evaluation of infants with bronchopulmonary dysplasia using cardiac catheterization. Pediatrics. 1982. 70:708–712.14. Mourani PM, Sontag MK, Younoszai A, Ivy DD, Abman SH. Clinical utility of echocardiography for the diagnosis and management of pulmonary vascular disease in young children with chronic lung disease. Pediatrics. 2008. 121:317–325.15. Kim HW, Kim GB, Je HG, et al. Pulmonary arterial hypertension in children: a single center experience. Korean Circ J. 2008. 38:644–650.16. Bossone E, Bodini BD, Mazza A, Allegra L. Pulmonary arterial hypertension: the key role of echocardiography. Chest. 2005. 127:1836–1843.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathophysiology and Risk Factors of Pulmonary Hypertension in Infants with Bronchopulmonary Dysplasia
- Survival of the Infants with Bronchopulmonary Dysplasia and Congenital Heart Disease
- Clinical Characteristics, Presentation, and Outcomes of Bronchopulmonary Dysplasia-Associated Pulmonary Hypertension
- Use of Inhaled Iloprost in an Infant With Bronchopulmonary Dysplasia and Pulmonary Artery Hypertension
- Optimal Ventilatory Strategies in Preterm Infants: Permissive Hypercapnia