Korean J Obstet Gynecol.
2012 May;55(5):293-299. 10.5468/KJOG.2012.55.5.293.
The risk factor related with small for gestational age in term delivery women with an episode of preterm labor
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. 20080251@kuh.ac.kr
- KMID: 2078144
- DOI: http://doi.org/10.5468/KJOG.2012.55.5.293
Abstract
OBJECTIVE
The aim of this study was to investigate the potential prognostic factors and it's relating factors of patients who were hospitalized for management of preterm labor.
METHODS
In this study, we retrospectively reviewed the records of 249 mothers who experienced the admission of preterm labor and delivered single live birth from January 2005 to May 2011 at our hospital. For our analyses, the mothers were divided into two groups according to delivery age; preterm birth group and full term birth group. And full term birth group was divided into two groups which had poor prognostic factors and compared with each other groups.
RESULTS
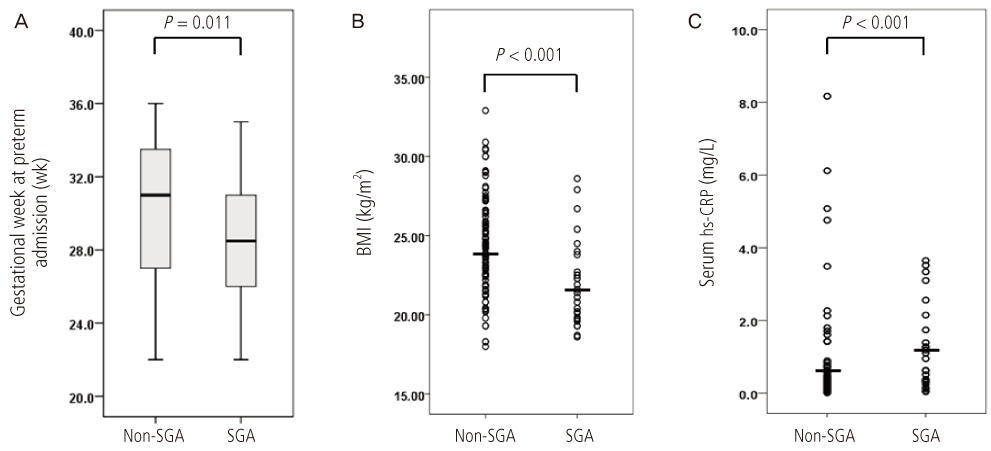
In our cohort, there was high incidence of small for gestational age in full term birth group compared with preterm birth group significantly (19.6% vs. 9.4%; P=0.028). And potential factors related to small for gestational age in full term birth group were early gestational age at 1st admission, low body mass index (BMI) in mothers and high highly sensitive C-reactive protein (hs-CRP) at 1st admission.
CONCLUSION
Gestational age at 1st admission, mother's BMI and hs-CRP at admission were significantly related to small for gestational age in full term birth who were hospitalized for management of preterm labor.
MeSH Terms
Figure
Cited by 1 articles
-
Does a preterm labor-assessment algorithm improve preterm labor-related knowledge, clinical practice confidence, and educational satisfaction?: a quasi-experimental study
Hee-Young Choi, Jeung-Im Kim
Korean J Women Health Nurs. 2023;29(3):219-228. doi: 10.4069/kjwhn.2023.08.17.
Reference
-
1. Kramer MS, Demissie K, Yang H, Platt RW, Sauvé R, Liston R. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. The contribution of mild and moderate preterm birth to infant mortality. JAMA. 2000. 284:843–849.2. Andrews WW, Hauth JC, Goldenberg RL. Infection and preterm birth. Am J Perinatol. 2000. 17:357–365.3. Gonik B, Creasy RK. Preterm labor: its diagnosis and management. Am J Obstet Gynecol. 1986. 154:3–8.4. Grover CM, Posner S, Kupperman M, Washington EA. Term delivery after hospitalization for preterm labor: incidence and costs in california. Prim Care Update Ob Gyns. 1998. 5:178.5. Kim YM, Bujold E, Chaiworapongsa T, Gomez R, Yoon BH, Thaler HT, et al. Failure of physiologic transformation of the spiral arteries in patients with preterm labor and intact membranes. Am J Obstet Gynecol. 2003. 189:1063–1069.6. Espinoza J, Kusanovic JP, Kim CJ, Kim YM, Kim JS, Hassan SS, et al. An episode of preterm labor is a risk factor for the birth of a small-for-gestational-age neonate. Am J Obstet Gynecol. 2007. 196:574.e1-e5.7. Imdad A, Yakoob MY, Siddiqui S, Bhutta ZA. Screening and triage of intrauterine growth restriction (IUGR) in general population and high risk pregnancies: a systematic review with a focus on reduction of IUGR related stillbirths. BMC Public Health. 2011. 11:Suppl 3. S1.8. Wang KG, Chen CP, Yang JM, Su TH. Impact of reverse end-diastolic flow velocity in umbilical artery on pregnancy outcome after the 28th gestational week. Acta Obstet Gynecol Scand. 1998. 77:527–531.9. Gortner L, Wauer RR, Stock GJ, Reiter HL, Reiss I, Jorch G, et al. Neonatal outcome in small for gestational age infants: do they really better? J Perinat Med. 1999. 27:484–489.10. Leitner Y, Fattal-Valevski A, Geva R, Eshel R, Toledano-Alhadef H, Rotstein M, et al. Neurodevelopmental outcome of children with intrauterine growth retardation: a longitudinal, 10-year prospective study. J Child Neurol. 2007. 22:580–587.11. Barker DJ. Adult consequences of fetal growth restriction. Clin Obstet Gynecol. 2006. 49:270–283.12. Janeway CA, Travers P, Walport M, Shlomchik MJ. Immunobiology: the immune system in health and disease. 2001. 5th ed. New York (NY): Garland Science.13. Cermak J, Key NS, Bach RR, Balla J, Jacob HS, Vercellotti GM. C-reactive protein induces human peripheral blood monocytes to synthesize tissue factor. Blood. 1993. 82:513–520.14. Burlingame RW, Volzer MA, Harris J, Du Clos TW. The effect of acute phase proteins on clearance of chromatin from the circulation of normal mice. J Immunol. 1996. 156:4783–4788.15. Ahmed N, Thorley R, Xia D, Samols D, Webster RO. Transgenic mice expressing rabbit C-reactive protein exhibit diminished chemotactic factor-induced alveolitis. Am J Respir Crit Care Med. 1996. 153:1141–1147.16. Belo L, Santos-Silva A, Rocha S, Caslake M, Cooney J, Pereira-Leite L, et al. Fluctuations in C-reactive protein concentration and neutrophil activation during normal human pregnancy. Eur J Obstet Gynecol Reprod Biol. 2005. 123:46–51.17. Sacks GP, Seyani L, Lavery S, Trew G. Maternal C-reactive protein levels are raised at 4 weeks gestation. Hum Reprod. 2004. 19:1025–1030.18. Romem Y, Artal R. C-reactive protein in pregnancy and in the postpartum period. Am J Obstet Gynecol. 1985. 151:380–383.19. Amarilyo G, Oren A, Mimouni FB, Ochshorn Y, Deutsch V, Mandel D. Increased cord serum inflammatory markers in small-for-gestational-age neonates. J Perinatol. 2011. 31:30–32.20. Rode L, Hegaard HK, Kjaergaard H, Moller LF, Tabor A, Ottesen B. Association between maternal weight gain and birth weight. Obstet Gynecol. 2007. 109:1309–1315.21. Beyerlein A, Schiessl B, Lack N, von Kries R. Associations of gestational weight loss with birth-related outcome: a retrospective cohort study. BJOG. 2011. 118:55–61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Value of Transvaginal Ultrasonographic Measurement of Cervical Length for Prediction of Preterm Delivery in Patients with Preterm Labor
- Efficacy of Fibronectin in Cervical Secretions, Measurement of Cervical Length & Shape by Transvaginal Sonography and Vaginal Swab PCR in Preterm Labor: Useful Predictor of Preterm Delivery
- Expression of Tissue Tissue-transglutaminase-2 (TGM2) and Cyclo-oxygenase (COX) in the Fetal Membrane of Preterm Birth
- Transvaginal Ultrasonographic Assessment of Cervical Length for Prediction of Preterm Delivery within 7 Days in Patients with Preterm Labor
- Efficacy of Maternal Serum Corticotropin Releasing Factor Levels in Diagnosis of Pregnancies Complicated by Preterm Labor