Painful Boney Metastases
- Affiliations
-
- 1Department of Anesthesiology, Albany Medical College, Albany, New York, USA. MohsinI@mail.amc.edu
- KMID: 2074023
- DOI: http://doi.org/10.3344/kjp.2013.26.3.223
Abstract
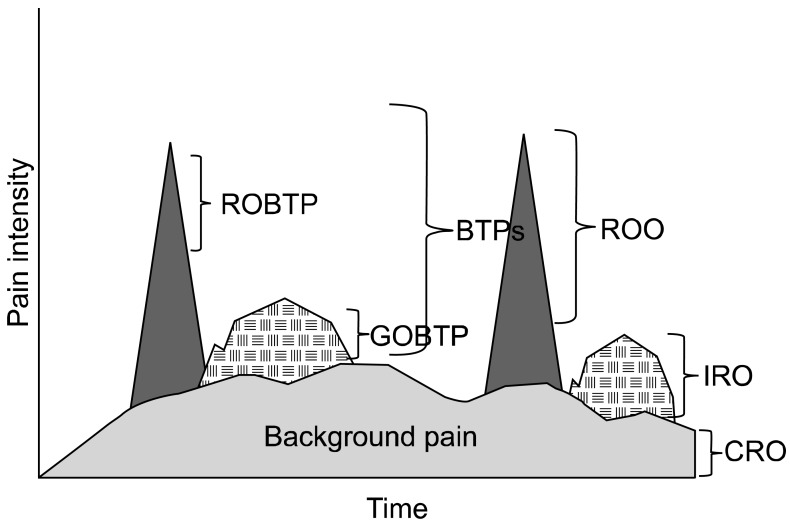
- Boney metastasis may lead to terrible suffering from debilitating pain. The most likely malignancies that spread to bone are prostate, breast, and lung. Painful osseous metastases are typically associated with multiple episodes of breakthrough pain which may occur with activities of daily living, weight bearing, lifting, coughing, and sneezing. Almost half of these breakthrough pain episodes are rapid in onset and short in duration and 44% of episodes are unpredictable. Treatment strategies include: analgesic approaches with "triple opioid therapy", bisphosphonates, chemotherapeutic agents, hormonal therapy, interventional and surgical approaches, steroids, radiation (external beam radiation, radiopharmaceuticals), ablative techniques (radiofrequency ablation, cryoablation), and intrathecal analgesics.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Extraspinal Percutaneous Osteoplasty for the Treatment of Painful Bony Metastasis
Jae-Heon Lee, Su-Young Kim, Hwoe-Gyeong Ok, Tae-Kyun Kim, Kyung-Hoon Kim
J Korean Med Sci. 2018;33(8):. doi: 10.3346/jkms.2018.33.e61.Tageted bipolar radiofrequency decompression with vertebroplasty for intractable radicular pain due to spinal metastasis: a case report
Seong Jin Baek, Hahck Soo Park, Eun Young Lee
Korean J Anesthesiol. 2016;69(4):395-399. doi: 10.4097/kjae.2016.69.4.395.Radiofrequency Thermal Ablation in Painful Myeloma of the Clavicle
Helen Gharaei, Farnad Imani, Masoud Vakily
Korean J Pain. 2014;27(1):72-76. doi: 10.3344/kjp.2014.27.1.72.Octanoic acid-rich diet alleviates breast cancer-induced bone pain
via the acyl-ghrelin/NPY pathway
Longjie Xu, Lili Hou, Chun Cao, Xiaohua Li
Korean J Pain. 2025;38(2):138-151. doi: 10.3344/kjp.24388.
Reference
-
1. Boyle P, Levin B. International Agency for Research on Cancer. World Health Organization. World cancer report 2008. Lyon: International Agency for Research on Cancer;2008.2. Berruti A, Dogliotti L, Bitossi R, Fasolis G, Gorzegno G, Bellina M, et al. Incidence of skeletal complications in patients with bone metastatic prostate cancer and hormone refractory disease: predictive role of bone resorption and formation markers evaluated at baseline. J Urol. 2000; 164:1248–1253. PMID: 10992374.
Article3. Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001; 93:247–257. PMID: 11514084.
Article4. van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007; 18:1437–1449. PMID: 17355955.
Article5. van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. High prevalence of pain in patients with cancer in a large population-based study in The Netherlands. Pain. 2007; 132:312–320. PMID: 17916403.
Article6. Laird BJ, Walley J, Murray GD, Clausen E, Colvin LA, Fallon MT. Characterization of cancer-induced bone pain: an exploratory study. Support Care Cancer. 2011; 19:1393–1401. PMID: 20680354.
Article7. Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997; 69:1–18. PMID: 9060007.
Article8. Delaney A, Fleetwood-Walker SM, Colvin LA, Fallon M. Translational medicine: cancer pain mechanisms and management. Br J Anaesth. 2008; 101:87–94. PMID: 18492671.
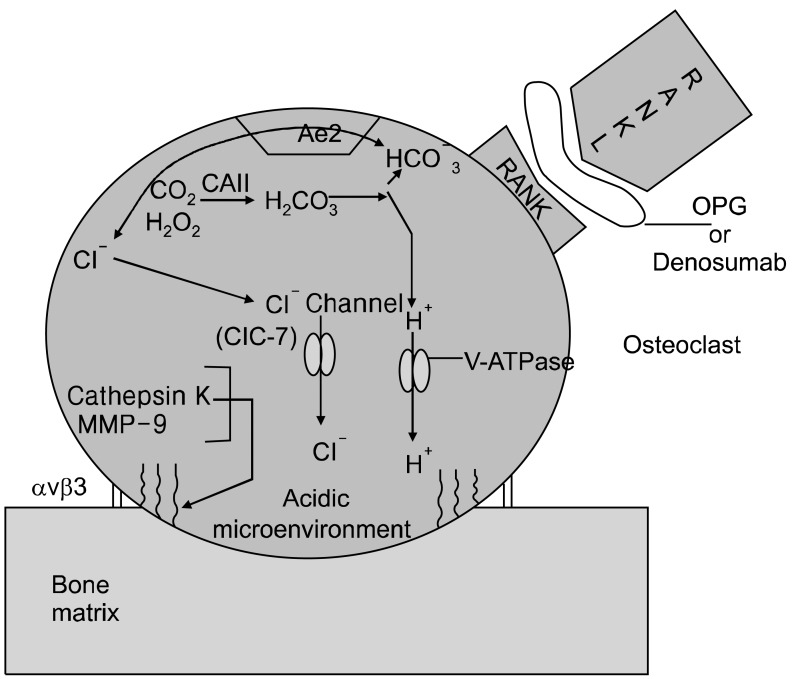
Article9. Saftig P, Hunziker E, Wehmeyer O, Jones S, Boyde A, Rommerskirch W, et al. Impaired osteoclastic bone resorption leads to osteopetrosis in cathepsin-K-deficient mice. Proc Natl Acad Sci U S A. 1998; 95:13453–13458. PMID: 9811821.
Article10. Everts V, Delaissé JM, Korper W, Jansen DC, Tigchelaar-Gutter W, Saftig P, et al. The bone lining cell: its role in cleaning Howship's lacunae and initiating bone formation. J Bone Miner Res. 2002; 17:77–90. PMID: 11771672.
Article11. Sly WS, Hewett-Emmett D, Whyte MP, Yu YS, Tashian RE. Carbonic anhydrase II deficiency identified as the primary defect in the autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcification. Proc Natl Acad Sci U S A. 1983; 80:2752–2756. PMID: 6405388.
Article12. Josephsen K, Praetorius J, Frische S, Gawenis LR, Kwon TH, Agre P, et al. Targeted disruption of the Cl-/HCO3- exchanger Ae2 results in osteopetrosis in mice. Proc Natl Acad Sci U S A. 2009; 106:1638–1641. PMID: 19164575.
Article13. Frattini A, Orchard PJ, Sobacchi C, Giliani S, Abinun M, Mattsson JP, et al. Defects in TCIRG1 subunit of the vacuolar proton pump are responsible for a subset of human autosomal recessive osteopetrosis. Nat Genet. 2000; 25:343–346. PMID: 10888887.
Article14. Karsdal MA, Henriksen K, Sørensen MG, Gram J, Schaller S, Dziegiel MH, et al. Acidification of the osteoclastic resorption compartment provides insight into the coupling of bone formation to bone resorption. Am J Pathol. 2005; 166:467–476. PMID: 15681830.
Article15. Baron R, Neff L, Louvard D, Courtoy PJ. Cell-mediated extracellular acidification and bone resorption: evidence for a low pH in resorbing lacunae and localization of a 100-kD lysosomal membrane protein at the osteoclast ruffled border. J Cell Biol. 1985; 101:2210–2222. PMID: 3905822.
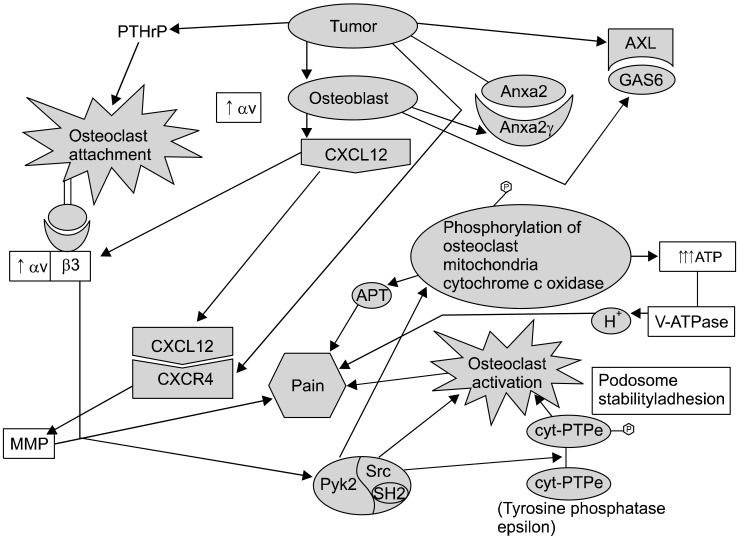
Article16. Miyazaki T, Tanaka S, Sanjay A, Baron R. The role of c-Src kinase in the regulation of osteoclast function. Mod Rheumatol. 2006; 16:68–74. PMID: 16633924.
Article17. Bradt J, Dileo C, Grocke D, Magill L. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev. 2011; (8):CD006911. PMID: 21833957.
Article18. Jane SW, Chen SL, Wilkie DJ, Lin YC, Foreman SW, Beaton RD, et al. Effects of massage on pain, mood status, relaxation, and sleep in Taiwanese patients with metastatic bone pain: a randomized clinical trial. Pain. 2011; 152:2432–2442. PMID: 21802850.
Article19. Burton AW, Cleeland CS. Cancer pain: progress since the WHO guidelines. Pain Pract. 2001; 1:236–242. PMID: 17134407.
Article20. Zech DF, Grond S, Lynch J, Hertel D, Lehmann KA. Validation of World Health Organization Guidelines for cancer pain relief: a 10-year prospective study. Pain. 1995; 63:65–76. PMID: 8577492.
Article21. Mercadante S. Intravenous morphine for management of cancer pain. Lancet Oncol. 2010; 11:484–489. PMID: 20434717.
Article22. Vielhaber A, Portenoy RK. Advances in cancer pain management. Hematol Oncol Clin North Am. 2002; 16:527–541. PMID: 12170566.
Article23. Urch C. The pathophysiology of cancer-induced bone pain: current understanding. Palliat Med. 2004; 18:267–274. PMID: 15198116.
Article24. Eisenberg E, Berkey CS, Carr DB, Mosteller F, Chalmers TC. Efficacy and safety of nonsteroidal antiinflammatory drugs for cancer pain: a meta-analysis. J Clin Oncol. 1994; 12:2756–2765. PMID: 7989953.
Article25. Levick S, Jacobs C, Loukas DF, Gordon DH, Meyskens FL, Uhm K. Naproxen sodium in treatment of bone pain due to metastatic cancer. Pain. 1988; 35:253–258. PMID: 3226754.
Article26. Stambaugh JE Jr, Drew J. The combination of ibuprofen and oxycodone/acetaminophen in the management of chronic cancer pain. Clin Pharmacol Ther. 1988; 44:665–669. PMID: 2461823.
Article27. Sacchetti G, Camera P, Rossi AP, Martoni A, Bruni G, Pannuti F. Injectable ketoprofen vs. acetylsalicylic acid for the relief of severe cancer pain: a double-blind, crossover trial. Drug Intell Clin Pharm. 1984; 18:403–406. PMID: 6373214.
Article28. McNicol E, Strassels SA, Goudas L, Lau J, Carr DB. NSAIDS or paracetamol, alone or combined with opioids, for cancer pain. Cochrane Database Syst Rev. 2005; (1):CD005180. PMID: 15654708.
Article29. Sheng H, Shao J, Kirkland SC, Isakson P, Coffey RJ, Morrow J, et al. Inhibition of human colon cancer cell growth by selective inhibition of cyclooxygenase-2. J Clin Invest. 1997; 99:2254–2259. PMID: 9151799.
Article30. Sabino MA, Ghilardi JR, Jongen JL, Keyser CP, Luger NM, Mach DB, et al. Simultaneous reduction in cancer pain, bone destruction, and tumor growth by selective inhibition of cyclooxygenase-2. Cancer Res. 2002; 62:7343–7349. PMID: 12499278.31. Isono M, Suzuki T, Hosono K, Hayashi I, Sakagami H, Uematsu S, et al. Microsomal prostaglandin E synthase-1 enhances bone cancer growth and bone cancer-related pain behaviors in mice. Life Sci. 2011; 88:693–700. PMID: 21324324.
Article32. Bruera E, Roca E, Cedaro L, Carraro S, Chacon R. Action of oral methylprednisolone in terminal cancer patients: a prospective randomized double-blind study. Cancer Treat Rep. 1985; 69:751–754. PMID: 2410117.33. Cain DM, Wacnik PW, Turner M, Wendelschafer-Crabb G, Kennedy WR, Wilcox GL, et al. Functional interactions between tumor and peripheral nerve: changes in excitability and morphology of primary afferent fibers in a murine model of cancer pain. J Neurosci. 2001; 21:9367–9376. PMID: 11717370.
Article34. Peters CM, Ghilardi JR, Keyser CP, Kubota K, Lindsay TH, Luger NM, et al. Tumor-induced injury of primary afferent sensory nerve fibers in bone cancer pain. Exp Neurol. 2005; 193:85–100. PMID: 15817267.
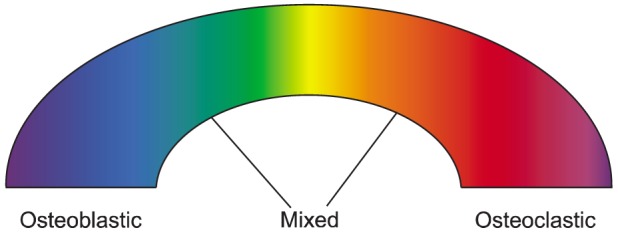
Article35. Halvorson KG, Sevcik MA, Ghilardi JR, Rosol TJ, Mantyh PW. Similarities and differences in tumor growth, skeletal remodeling and pain in an osteolytic and osteoblastic model of bone cancer. Clin J Pain. 2006; 22:587–600. PMID: 16926574.
Article36. Jimenez-Andrade JM, Mantyh P. Cancer pain: from the development of mouse models to human clinical trials. In : Kruger L, Light AR, editors. Translational pain research: from mouse to man. Boca Raton (FL): CRC Press;2010. p. 1–22.37. Donovan-Rodriguez T, Dickenson AH, Urch CE. Gabapentin normalizes spinal neuronal responses that correlate with behavior in a rat model of cancer-induced bone pain. Anesthesiology. 2005; 102:132–140. PMID: 15618797.
Article38. Caraceni A, Zecca E, Bonezzi C, Arcuri E, Yaya Tur R, Maltoni M, et al. Gabapentin for neuropathic cancer pain: a randomized controlled trial from the Gabapentin Cancer Pain Study Group. J Clin Oncol. 2004; 22:2909–2917. PMID: 15254060.
Article39. Caraceni A, Zecca E, Martini C, Pigni A, Bracchi P. Gabapentin for breakthrough pain due to bone metastases. Palliat Med. 2008; 22:392–393. PMID: 18541644.
Article40. Kato A, Minami K, Ito H, Tomii T, Matsumoto M, Orita S, et al. Oxycodone-induced analgesic effects in a bone cancer pain model in mice. Oncology. 2008; 74(Suppl 1):55–60. PMID: 18758199.
Article41. Bailey F, Farley A. Oral opioid drugs. In : Davies A, editor. Cancer-related breakthrough pain. Oxford: Oxford University Press;2006. p. 43–55.42. Portenoy RK, Payne D, Jacobsen P. Breakthrough pain: characteristics and impact in patients with cancer pain. Pain. 1999; 81:129–134. PMID: 10353500.
Article43. Costa L, Major PP. Effect of bisphosphonates on pain and quality of life in patients with bone metastases. Nat Clin Pract Oncol. 2009; 6:163–174. PMID: 19190592.
Article44. Mönkkönen H, Auriola S, Lehenkari P, Kellinsalmi M, Hassinen IE, Vepsäläinen J, et al. A new endogenous ATP analog (ApppI) inhibits the mitochondrial adenine nucleotide translocase (ANT) and is responsible for the apoptosis induced by nitrogen-containing bisphosphonates. Br J Pharmacol. 2006; 147:437–445. PMID: 16402039.
Article45. Berenson JR, Hillner BE, Kyle RA, Anderson K, Lipton A, Yee GC, et al. American Society of Clinical Oncology clinical practice guidelines: the role of bisphosphonates in multiple myeloma. J Clin Oncol. 2002; 20:3719–3736. PMID: 12202673.
Article46. Pistevou-Gombaki K, Eleftheriadis N, Sofroniadis I, Makris P, Kouloulias V. Palliative treatment of painful bone metastases from non-Hodgkin lymphoma with disodium pamidronate. J Exp Clin Cancer Res. 2002; 21:429–432. PMID: 12385590.47. Santini D, Fratto ME, Vincenzi B, Galluzzo S, Tonini G. Zoledronic acid in the management of metastatic bone disease. Expert Opin Biol Ther. 2006; 6:1333–1348. PMID: 17223741.
Article48. Amir E, Whyne C, Freedman OC, Fralick M, Kumar R, Hardisty M, et al. Radiological changes following second-line zoledronic acid treatment in breast cancer patients with bone metastases. Clin Exp Metastasis. 2009; 26:479–484. PMID: 19266291.
Article49. Hiraga T, Williams PJ, Ueda A, Tamura D, Yoneda T. Zoledronic acid inhibits visceral metastases in the 4T1/luc mouse breast cancer model. Clin Cancer Res. 2004; 10:4559–4567. PMID: 15240548.
Article50. Furlow B. Zoledronic acid palliation in bone-metastatic breast cancer. Lancet Oncol. 2006; 7:894. PMID: 17099983.
Article51. Fulfaro F, Leto G, Badalamenti G, Arcara C, Cicero G, Valerio MR, et al. The use of zoledronic acid in patients with bone metastases from prostate carcinoma: effect on analgesic response and bone metabolism biomarkers. J Chemother. 2005; 17:555–559. PMID: 16323446.
Article52. Rachner TD, Singh SK, Schoppet M, Benad P, Bornhäuser M, Ellenrieder V, et al. Zoledronic acid induces apoptosis and changes the TRAIL/OPG ratio in breast cancer cells. Cancer Lett. 2010; 287:109–116. PMID: 19577359.
Article53. Woodward JK, Neville-Webbe HL, Coleman RE, Holen I. Combined effects of zoledronic acid and doxorubicin on breast cancer cell invasion in vitro. Anticancer Drugs. 2005; 16:845–854. PMID: 16096432.
Article54. Santini D, Vincenzi B, Galluzzo S, Battistoni F, Rocci L, Venditti O, et al. Repeated intermittent low-dose therapy with zoledronic acid induces an early, sustained, and long-lasting decrease of peripheral vascular endothelial growth factor levels in cancer patients. Clin Cancer Res. 2007; 13:4482–4486. PMID: 17671133.
Article55. Vincenzi B, Santini D, Dicuonzo G, Battistoni F, Gavasci M, La Cesa A, et al. Zoledronic acid-related angiogenesis modifications and survival in advanced breast cancer patients. J Interferon Cytokine Res. 2005; 25:144–151. PMID: 15767788.
Article56. Tong D, Gillick L, Hendrickson FR. The palliation of symptomatic osseous metastases: final results of the study by the Radiation Therapy Oncology Group. Cancer. 1982; 50:893–899. PMID: 6178497.
Article57. Arcangeli G, Micheli A, Arcangeli G, Giannarelli D, La Pasta O, Tollis A, et al. The responsiveness of bone metastases to radiotherapy: the effect of site, histology and radiation dose on pain relief. Radiother Oncol. 1989; 14:95–101. PMID: 2469105.
Article58. Dennis K, Wong K, Zhang L, Culleton S, Nguyen J, Holden L, et al. Palliative radiotherapy for bone metastases in the last 3 months of life: worthwhile or futile? Clin Oncol (R Coll Radiol). 2011; 23:709–715. PMID: 21665446.
Article59. Poulter CA, Cosmatos D, Rubin P, Urtasun R, Cooper JS, Kuske RR, et al. A report of RTOG 8206: a phase III study of whether the addition of single dose hemibody irradiation to standard fractionated local field irradiation is more effective than local field irradiation alone in the treatment of symptomatic osseous metastases. Int J Radiat Oncol Biol Phys. 1992; 23:207–214. PMID: 1374061.
Article60. Jeremic B. Single fraction external beam radiation therapy in the treatment of localized metastatic bone pain. A review. J Pain Symptom Manage. 2001; 22:1048–1058. PMID: 11738168.
Article61. Wu JS, Wong R, Johnston M, Bezjak A, Whelan T. Cancer Care Ontario Practice Guidelines Initiative Supportive Care Group. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys. 2003; 55:594–605. PMID: 12573746.
Article62. Sze WM, Shelley MD, Held I, Wilt TJ, Mason MD. Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy--a systematic review of randomised trials. Clin Oncol (R Coll Radiol). 2003; 15:345–352. PMID: 14524489.
Article63. Chow E, Harris K, Fan G, Tsao M, Sze WM. Palliative radiotherapy trials for bone metastases: a systematic review. J Clin Oncol. 2007; 25:1423–1436. PMID: 17416863.
Article64. Rades D, Schild SE, Abrahm JL. Treatment of painful bone metastases. Nat Rev Clin Oncol. 2010; 7:220–229. PMID: 20234353.
Article65. Nomiya T, Teruyama K, Wada H, Nemoto K. Time course of pain relief in patients treated with radiotherapy for cancer pain: a prospective study. Clin J Pain. 2010; 26:38–42. PMID: 20026951.
Article66. Huisman M, van den Bosch MA, Wijlemans JW, van Vulpen M, van der Linden YM, Verkooijen HM. Effectiveness of reirradiation for painful bone metastases: a systematic review and meta-analysis. Int J Radiat Oncol Biol Phys. 2012; 84:8–14. PMID: 22300568.
Article67. Smith H, Navani A, Fishman SM. Radiopharmaceuticals for palliation of painful osseous metastases. Am J Hosp Palliat Care. 2004; 21:303–313. PMID: 15315195.
Article68. Roqué I Figuls M, Martinez-Zapata MJ, Scott-Brown M, Alonso-Coello P. Radioisotopes for metastatic bone pain. Cochrane Database Syst Rev. 2011; (7):CD003347. PMID: 21735393.
Article69. Paes FM, Serafini AN. Systemic metabolic radiopharmaceutical therapy in the treatment of metastatic bone pain. Semin Nucl Med. 2010; 40:89–104. PMID: 20113678.
Article70. Robinson RG, Preston DF, Spicer JA, Baxter KG. Radionuclide therapy of intractable bone pain: emphasis on strontium-89. Semin Nucl Med. 1992; 22:28–32. PMID: 1589803.
Article71. Finlay IG, Mason MD, Shelley M. Radioisotopes for the palliation of metastatic bone cancer: a systematic review. Lancet Oncol. 2005; 6:392–400. PMID: 15925817.
Article72. Samarium-153 lexidronam for painful bone metastases. Med Lett Drugs Ther. 39:1997; 83–84. PMID: 9286284.73. Alberts AS, Smit BJ, Louw WK, van Rensburg AJ, van Beek A, Kritzinger V, et al. Dose response relationship and multiple dose efficacy and toxicity of samarium-153-EDTMP in metastatic cancer to bone. Radiother Oncol. 1997; 43:175–179. PMID: 9192964.
Article74. Sartor O, Reid RH, Bushnell DL, Quick DP, Ell PJ. Safety and efficacy of repeat administration of samarium Sm-153 lexidronam to patients with metastatic bone pain. Cancer. 2007; 109:637–643. PMID: 17167764.
Article75. Nazario J, Hernandez J, Tam AL. Thermal ablation of painful bone metastases. Tech Vasc Interv Radiol. 2011; 14:150–159. PMID: 21767782.
Article76. Callstrom MR, Charboneau JW. Image-guided palliation of painful metastases using percutaneous ablation. Tech Vasc Interv Radiol. 2007; 10:120–131. PMID: 18070690.
Article77. Di Staso M, Zugaro L, Gravina GL, Bonfili P, Marampon F, Di Nicola L, et al. A feasibility study of percutaneous radiofrequency ablation followed by radiotherapy in the management of painful osteolytic bone metastases. Eur Radiol. 2011; 21:2004–2010. PMID: 21533865.
Article78. Dupuy DE, Hong R, Oliver B, Goldberg SN. Radiofrequency ablation of spinal tumors: temperature distribution in the spinal canal. AJR Am J Roentgenol. 2000; 175:1263–1266. PMID: 11044019.79. Tancioni F, Lorenzetti MA, Navarria P, Pessina F, Draghi R, Pedrazzoli P, et al. Percutaneous vertebral augmentation in metastatic disease: state of the art. J Support Oncol. 2011; 9:4–10. PMID: 21465731.
Article80. Peh WC, Gilula LA. Percutaneous vertebroplasty: indications, contraindications, and technique. Br J Radiol. 2003; 76:69–75. PMID: 12595329.
Article81. Lee B, Franklin I, Lewis JS, Coombes RC, Leonard R, Gishen P, et al. The efficacy of percutaneous vertebroplasty for vertebral metastases associated with solid malignancies. Eur J Cancer. 2009; 45:1597–1602. PMID: 19223174.
Article82. Saliou G, Kocheida el M, Lehmann P, Depriester C, Paradot G, Le Gars D, et al. Percutaneous vertebroplasty for pain management in malignant fractures of the spine with epidural involvement. Radiology. 2010; 254:882–890. PMID: 20177099.
Article83. Kassamali RH, Ganeshan A, Hoey ET, Crowe PM, Douis H, Henderson J. Pain management in spinal metastases: the role of percutaneous vertebral augmentation. Ann Oncol. 2011; 22:782–786. PMID: 20966180.
Article84. Qian Z, Sun Z, Yang H, Gu Y, Chen K, Wu G. Kyphoplasty for the treatment of malignant vertebral compression fractures caused by metastases. J Clin Neurosci. 2011; 18:763–767. PMID: 21507652.
Article85. Smith TJ, Staats PS, Deer T, Stearns LJ, Rauck RL, Boortz-Marx RL, et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol. 2002; 20:4040–4049. PMID: 12351602.
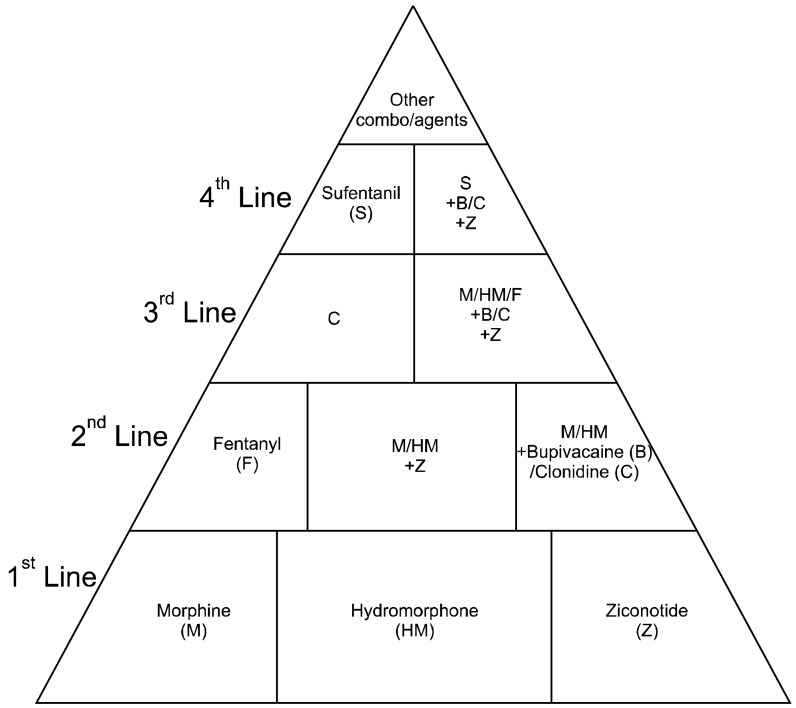
Article86. Deer T, Krames ES, Hassenbusch SJ, Burton A, Caraway D, Dupen S, et al. Polyanalgesic consensus conference 2007: recommendations for the management of pain by intrathecal (intraspinal) drug delivery: report of an interdisciplinary expert panel. Neuromodulation. 2007; 10:300–328. PMID: 22150890.
Article87. Deer TR, Smith HS, Burton AW, Pope JE, Doleys DM, Levy RM, et al. Comprehensive consensus based guidelines on intrathecal drug delivery systems in the treatment of pain caused by cancer pain. Pain Physician. 2011; 14:E283–E312. PMID: 21587338.88. Papachristou DJ, Basdra EK, Papavassiliou AG. Bone metastases: molecular mechanisms and novel therapeutic interventions. Med Res Rev. 2012; 32:611–636. PMID: 20818675.
Article89. Kong YY, Feige U, Sarosi I, Bolon B, Tafuri A, Morony S, et al. Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature. 1999; 402:304–309. PMID: 10580503.
Article90. Hsu H, Lacey DL, Dunstan CR, Solovyev I, Colombero A, Timms E, et al. Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc Natl Acad Sci U S A. 1999; 96:3540–3545. PMID: 10097072.
Article91. Body JJ, Greipp P, Coleman RE, Facon T, Geurs F, Fermand JP, et al. A phase I study of AMGN-0007, a recombinant osteoprotegerin construct, in patients with multiple myeloma or breast carcinoma related bone metastases. Cancer. 2003; 97:887–892. PMID: 12548591.
Article92. Schwarz EM, Ritchlin CT. Clinical development of anti-RANKL therapy. Arthritis Res Ther. 2007; 9(Suppl 1):S7. PMID: 17634146.
Article93. Kaan TK, Yip PK, Patel S, Davies M, Marchand F, Cockayne DA, et al. Systemic blockade of P2X3 and P2X2/3 receptors attenuates bone cancer pain behaviour in rats. Brain. 2010; 133:2549–2564. PMID: 20802203.
Article94. Chen J, Wang L, Zhang Y, Yang J. P2Y1 purinoceptor inhibition reduces extracellular signal-regulated protein kinase 1/2 phosphorylation in spinal cord and dorsal root ganglia: implications for cancer-induced bone pain. Acta Biochim Biophys Sin (Shanghai). 2012; 44:367–372. PMID: 22349022.
Article95. Tomura H, Mogi C, Sato K, Okajima F. Proton-sensing and lysolipid-sensitive G-protein-coupled receptors: a novel type of multi-functional receptors. Cell Signal. 2005; 17:1466–1476. PMID: 16014326.
Article96. Huang CW, Tzeng JN, Chen YJ, Tsai WF, Chen CC, Sun WH. Nociceptors of dorsal root ganglion express proton-sensing G-protein-coupled receptors. Mol Cell Neurosci. 2007; 36:195–210. PMID: 17720533.
Article97. Chen YJ, Huang CW, Lin CS, Chang WH, Sun WH. Expression and function of proton-sensing G-protein-coupled receptors in inflammatory pain. Mol Pain. 2009; 5:39. PMID: 19602228.
Article98. Pérez-Sayáns M, Somoza-Martín JM, Barros-Angueira F, Rey JM, García-García A. V-ATPase inhibitors and implication in cancer treatment. Cancer Treat Rev. 2009; 35:707–713. PMID: 19758758.
Article99. Reeh PW, Steen KH. Tissue acidosis in nociception and pain. Prog Brain Res. 1996; 113:143–151. PMID: 9009732.100. Sin WC, Zhang Y, Zhong W, Adhikarakunnathu S, Powers S, Hoey T, et al. G protein-coupled receptors GPR4 and TDAG8 are oncogenic and overexpressed in human cancers. Oncogene. 2004; 23:6299–6303. PMID: 15221007.
Article101. Hang LH, Yang JP, Yin W, Wang LN, Guo F, Ji FH, et al. Activation of spinal TDAG8 and its downstream PKA signaling pathway contribute to bone cancer pain in rats. Eur J Neurosci. 2012; 36:2107–2117. PMID: 22515300.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pallative effect of radiation therapy in management of symptomatic osseous metastases
- Percutaneous Sacroplasty for Painful Sacral Metastases Involving Multiple Sacral Vertebral Bodies: Initial Experience with an Interpedicular Approach
- Palliative Radiotherapy for Painful Bone Metastases
- Multiple Solitary Plasmacytomas Presenting with Painful Erythematous Swelling of the Upper Eyelid
- Percutaneous osteoplasty for painful bony lesions: a technical survey