Korean J Perinatol.
2013 Dec;24(4):300-305. 10.14734/kjp.2013.24.4.300.
A Case of Non-Immune Hydrops Fetalis due to Umbilical Venous Malformation and Noonan Syndrome
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. lamb4122@snu.ac.kr
- KMID: 2072307
- DOI: http://doi.org/10.14734/kjp.2013.24.4.300
Abstract
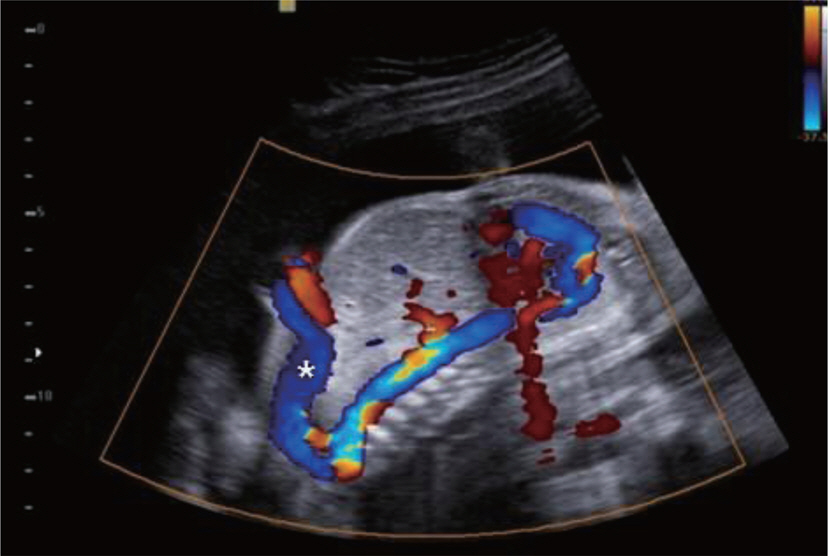
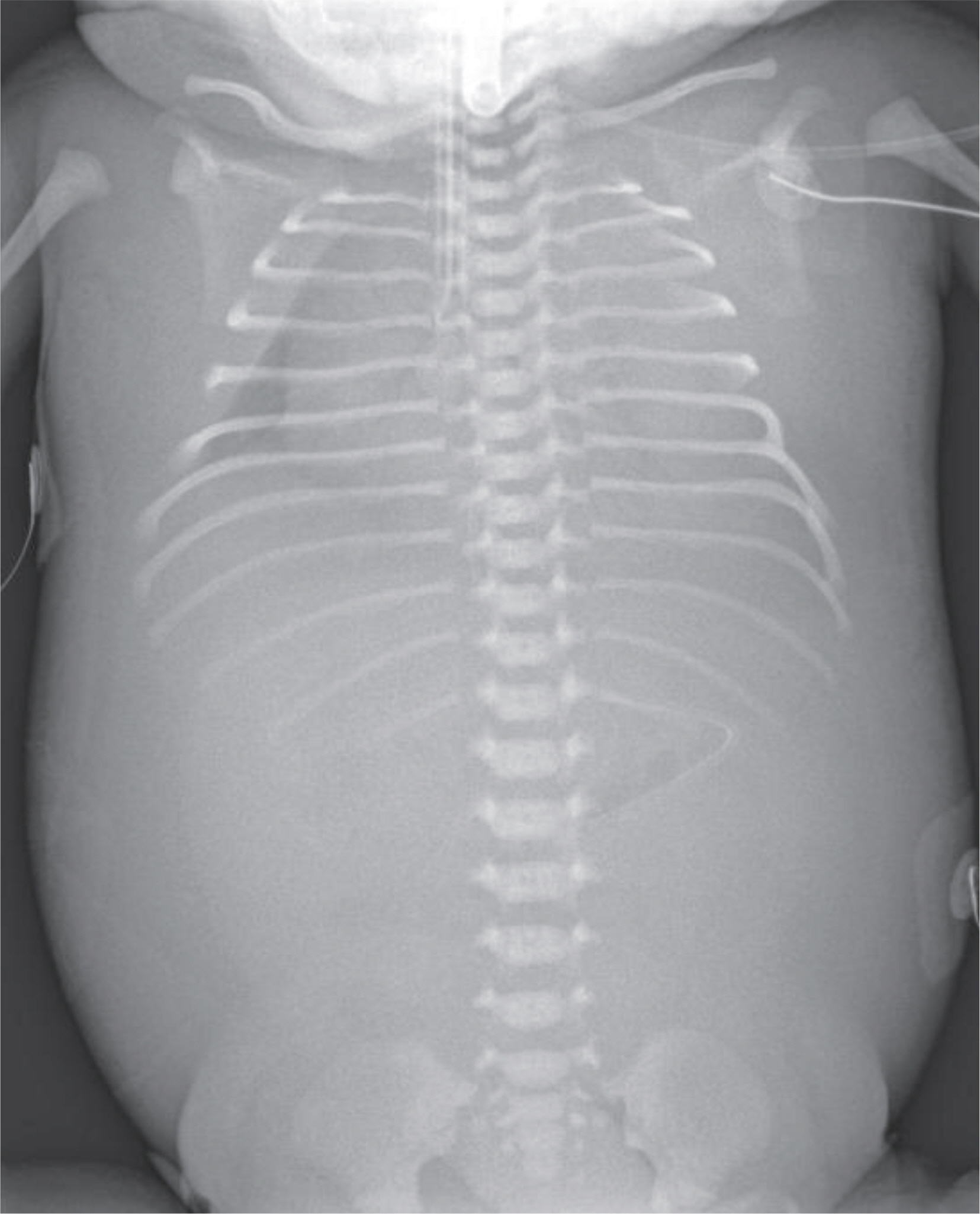
- Anomalies of the fetal venous system are rare. Major portion of fetal venous anomalies are malformation of umbilical vein and ductus venosus. Abnormal umbilico-systemic shunt, bypassing the ductus venosus makes direct connection between the high-pressure umbilical system and the low-pressure systemic system. And it makes adverse to the fetal hemodynamics. Fetal hemodynamic distress may induce fetal growth retardation, hepatomegaly, cardiomegaly, hydrops fetalis and fetal death. We report a case of non-immune hydrops fetalis which was associated with abnormal umbilical vein pathway. Our patient had bifurcated umbilical veins. Main branch of umbilical vein was drained directly to the left internal iliac vein and another branch was drained to the portal vein. After birth, extrahepatic shunt through main branch of umbilical vein that bypassed the portal system was persisted and thrombocytopenia was combined due to consumption in thrombus of a dilated anomalous umbilical vein. Later this case was diagnosed as Noonan syndrome with a genetic testing.
MeSH Terms
Figure
Reference
-
1). Achiron R., Hegesh J., Yagel S., Lipitz S., Cohen SB., Rotstein Z. Abnormalities of the fetal central veins and umbilico-portal system: prenatal ultrasonographic diagnosis and proposed classification. Ultrasound Obstet Gynecol. 2000. 16:539–48.
Article2). Chung IB. Prenatal diagnosis of the fetal venous system abnormalities. Korean J Ultrasound Obstet Gynecol. 2009. 11:51–9.3). Fasouliotis SJ., Achiron R., Kivilevitch Z., Yagel S. The human fetal venous system - Normal embryologic, anatomic, and physiologic characteristics and developmental abnormalities. J Ultrasound Med. 2002. 21:1145–58.4). Hofstaetter C., Plath H., Hansmann M. Prenatal diagnosis of abnormalities of the fetal venous system. Ultrasound Obstet Gynecol. 2000. 15:231–41.
Article5). Passalacqua M., Lie KT., Yarmohammadi H. Congenital extrahepatic portosystemic shunt (Abernethy malformation) treated endovascularly with vascular plug shunt closure. Pediatr Surg Int. 2012. 28:79–83.
Article6). Gorincour G., Droulle P., Guibaud L. Prenatal diagnosis of umbilicoportosystemic shunts: report of 11 cases and review of the literature. AJR. 2005. 184:163–8.
Article7). Vanrykel K., Bruneel E., Van Hoestenberghe MR., Buekenhout L., Gyselaers W., Theyskens C. Neonatal disseminated intravascular coagulation after thrombosis of a fetal intraabdominal umbilical vein varix. J Obstet Gynaecol. 2010. 30:315.
Article8). De Catte L., Osmanagaoglu K., De Schrijver I. Persistent right umbilical vein in trisomy 18: sonographic observation. J Ultrasound Med. 1998. 17:775–9.
Article9). Wolman I., Gull I., Fait G., Amster R., Kupferminc MJ., Lessing JB, et al. Persistent right umbilical vein: incidence and significance. Ultrasound Obstet Gynecol. 2002. 19:562–4.
Article10). Currarino G., Stannard MW., Kolni H. Umbilical vein draining into the inferior vena cava via the internal iliac vein, bypassing the liver. Pediatr Radiol. 1991. 21:265–6.
Article11). Romano AA., Allanson JE., Dahlgren J., Gelb BD., Hall B., Pierpont ME, et al. Noonan syndrome: clinical features, diagnosis, and management guidelines. Pediatrics. 2010. 126:746–59.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Hydrops Fetalis due to Placental Chorangiomatosis
- A Case of Non-immune Hydrops Fetalis due to Congenital Syphilis
- Causes of Hydrops Fetalis: Analysis of 149 Autopsy Cases
- A Case of Non-immune Hydrops Fetalis due to Intraperitoneal Hemangioma
- A case of hydrops fetalis of the newborn due to anti-E