Korean J Perinatol.
2013 Dec;24(4):290-299. 10.14734/kjp.2013.24.4.290.
Respiratory Morbidities in Newborn Infants by Gestational Age Following Elective Cesarean Section beyond 35 Weeks of Gestation
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. kimek@snu.ac.kr
- KMID: 2072306
- DOI: http://doi.org/10.14734/kjp.2013.24.4.290
Abstract
- PURPOSE
We evaluate respiratory morbidities in infants beyond 35 weeks of gestation born via elective cesarean section by gestational age.
METHODS
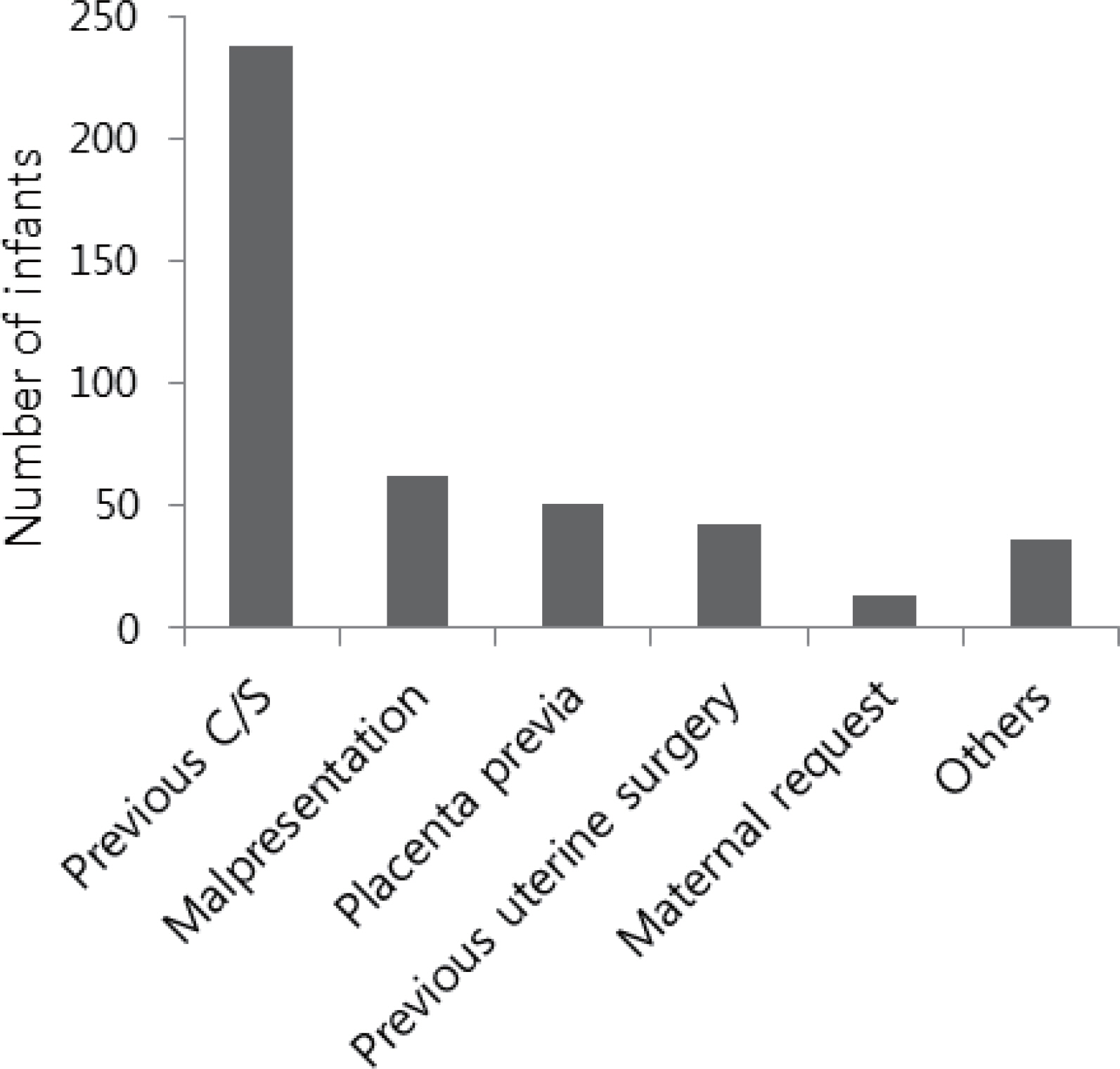
This is a retrospective study of 443 infants who were born at Seoul National University Hospital by elective cesarean section beyond 35 weeks of gestation from January 2011 to December 2012. We compared respiratory morbidities in four groups classified by gestational age (35(+0)-36(+6) weeks, 37(+0)-37(+6) weeks, 38(+0)-38(+6) weeks, 39(+0)-40(+6) weeks).
RESULTS
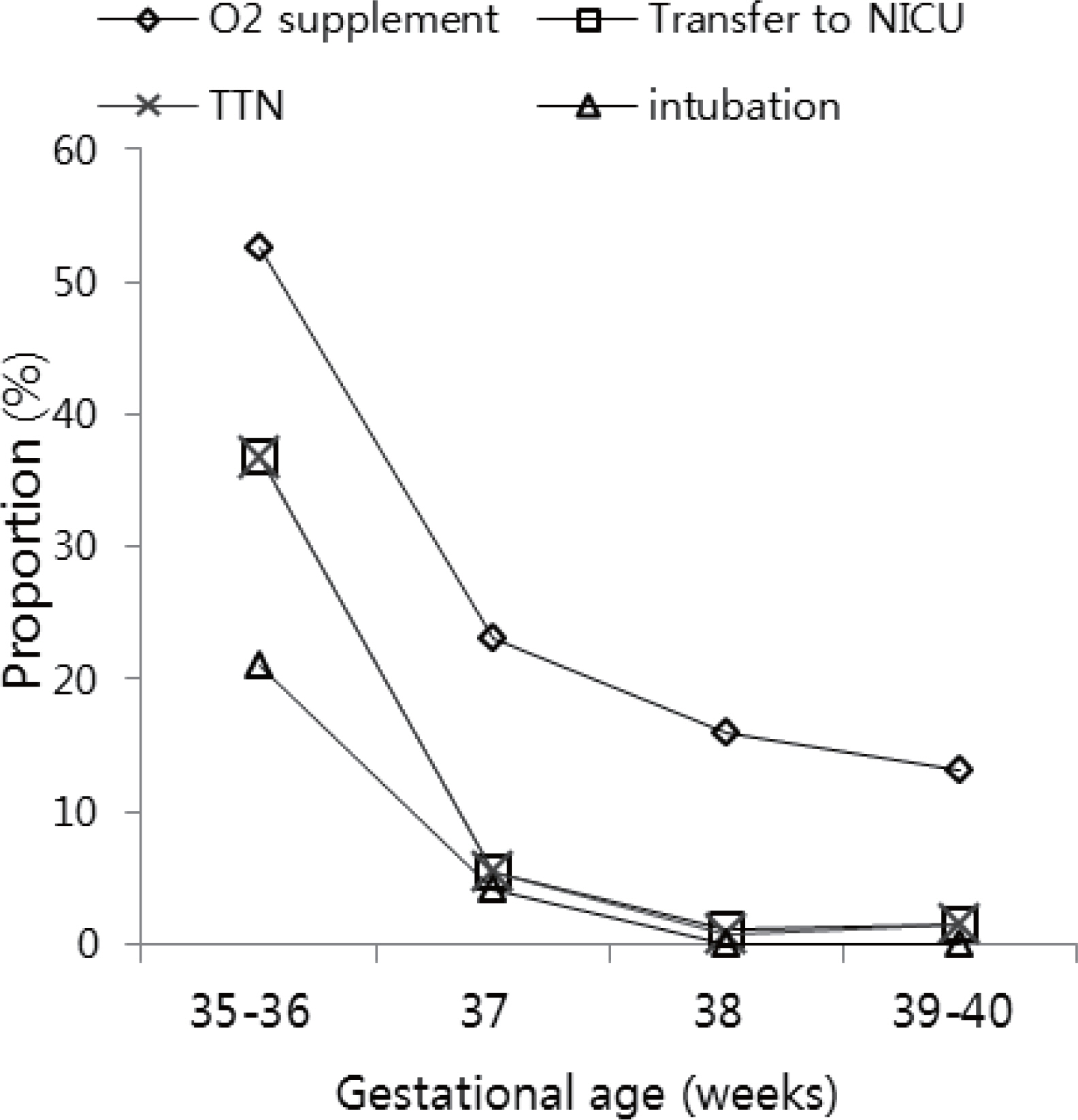
There were significantly lower Apgar scores in the late-preterm infant group (35-36 weeks) compared to other term infant groups and the proportion of infants born from mothers with preeclampsia gradually decreased as gestational age increased. There were significant differences in O2 supplement, duration of O2 (>24 hours), checked chest radiography, transient tachypnea of newborn (TTN), transfer to neonatal intensive care unit (NICU), endotracheal intubation, and ventilator uses including nasal continuous positive airway pressure in four groups (P<0.05). By logistic regression analysis, compared to births at 38 weeks, births at 35-36 weeks and at 37 weeks were associated with an increased risk of respiratory morbidities [odds ratios (OR) and 95% confidence intervals (CI) for births at 35-36 weeks, 122.5 (17.4-863.4) for TTN; 54.0 (10.1-289.4) for transfer to NICU; 99.5 (14.9-666.2) for ventilator apply; OR and 95% CI for births at 37 weeks, 8.8 (1.6-50.1) for TTN; 5.3 (1.1-24.7) for transfer to NICU; 8.4 (1.5-47.7) for ventilator apply; P<0.05]. There were no significant differences in respiratory morbidities between births at 38 weeks and births at 39-40 weeks.
CONCLUSION
Postponing the timing of elective cesarean section to beyond 38 weeks of gestation would be helpful in reducing the neonatal respiratory morbidities.
MeSH Terms
-
Cesarean Section*
Continuous Positive Airway Pressure
Female
Gestational Age*
Humans
Infant
Infant, Newborn*
Intensive Care, Neonatal
Intubation, Intratracheal
Logistic Models
Mothers
Parturition
Pre-Eclampsia
Pregnancy
Pregnancy*
Radiography
Respiration Disorders
Retrospective Studies
Seoul
Term Birth
Thorax
Transient Tachypnea of the Newborn
Ventilators, Mechanical
Figure
Reference
-
1). Martin JA., Hamilton BE., Ventura SJ., Osterman MJ., Kirmeyer S., Mathews TJ, et al. Births: final data for 2009. Natl Vital Stat Rep. 2011. 60:1–70.2). Gholitabar M., Ullman R., James D., Griffiths M. Caesarean section: summary of updated NICE guidance. BMJ. 2011. 343:d7108.
Article3). Korean Statistical Information Service. 2003 Survey on the national fertility, family health and welfare. Available from:. http://kosis.kr/.4). Korean Statistical Information Service. 2010 Cesarean Section Indicators by Type of Medical Care Institutions. Available from:. http://kosis.kr/.5). Jain L., Dudell GG. Respiratory transition in infants delivered by cesarean section. Semin Perinatol. 2006. 30:296–304.
Article6). Fogelson NS., Menard MK., Hulsey T., Ebeling M. Neonatal impact of elective repeat cesarean delivery at term: a comment on patient choice cesarean delivery. Am J Obstet Gynecol. 2005. 192:1433–6.
Article7). Hansen AK., Wisborg K., Uldbjerg N., Henriksen TB. Elective caesarean section and respiratory morbidity in the term and near-term neonate. Acta Obstet Gynecol Scand. 2007. 86:389–94.
Article8). Hansen AK., Wisborg K., Uldbjerg N., Henriksen TB. Risk of respiratory morbidity in term infants delivered by elective caesarean section: cohort study. BMJ. 2008. 336:85–7.
Article9). Zanardo V., Simbi AK., Franzoi M., Soldà G., Salvadori A., Trevisanuto D. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery. Acta Paediatr. 2004. 93:643–7.
Article10). Morrison JJ., Rennie JM., Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995. 102:101–6.
Article11). Hales KA., Morgan MA., Thurnau GR. Influence of labor and route of delivery on the frequency of respiratory morbidity in term neonates. Int J Gynaecol Obstet. 1993. 43:35–40.
Article12). Cohen M., Carson BS. Respiratory morbidity benefit of awaiting onset of labor after elective cesarean section. Obstet Gynecol. 1985. 65:818–24.
Article13). Tita ATN., Landon MB., Spong CY., Lai Y., Leveno KJ., Varner MW, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009. 360:111–20.
Article14). Wilmink FA., Hukkelhoven CWPM., Lunshof S., Mol BWJ., van der Post JAM., Papatsonis DNM. Neonatal outcome following elective cesarean section beyond 37 weeks of gestation: a 7-year retrospective analysis of a national registry. Am J Obstet Gynecol. 2010. 202:250. .e1-8.
Article15). Hibbard JU., Wilkins I., Sun L., Gregory K., Haberman S., Hoffman M, et al. Respiratory morbidity in late preterm births. JAMA. 2010. 304:419–25.
Article16). Choi S., Kim S., Oh J., Lee N., Kim S., Kim M, et al. The Respiratory Morbidities in Late-preterm Infants Compared with the Early-preterm and Term Infants throughout the First Year of Life. J Korean Soc Neonatol. 2012. 19:245–52.
Article17). Gouyon JB., Ribakovsky C., Ferdynus C., Quantin C., Sagot P., Gouyon B, et al. Severe respiratory disorders in term neonates. Paediatr Perinat Epidemiol. 2008. 22:22–30.
Article18). Wax JR., Herson V., Carignan E., Mather J., Ingardia CJ. Contribution of elective delivery to severe respiratory distress at term. Am J Perinatol. 2002. 19:81–6.
Article19). van den Berg A., van Elburg RM., van Geijn HP., Fetter WP. Neonatal respiratory morbidity following elective caesarean section in term infants. A 5-year retrospective study and a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2001. 98:9–13.20). Hourani M., Ziade F., Rajab M. Timing of planned caesarean section and the morbidities of the newborn. N Am J Med Sci. 2011. 3:465–8.
Article21). American College of Obstetricians and Gynecologists. ACOG committee opinion no. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013. 121:911–5.22). American College of Obstetricians and Gynecologists. ACOG committee opinion no. 559: Cesarean delivery on maternal request. Obstet Gynecol. 2013. 121:904–7.23). National Institute for Health and Clinical Excellence. Caesarean section (update). NICE clinical guideline 132. 2011. Available from:. http://guidance.nice.org.uk/CG132.24). Rugolo LMSdS. Bentlin MR., Trindade CEP. Preeclampsia Early and Late Neonatal Outcomes. Neoreviews. 2012. 13:e532–41.25). Turner JA. Diagnosis and management of pre-eclampsia: an update. Int J Womens Health. 2010. 2:327–37.
Article26). American College of Obstetricians and Gynecologists. ACOG committee opinion no. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013. 121:908–10.27). Stutchfield P., Whitaker R., Russell I. Antenatal betamethasone and incidence of neonatal respiratory distress after elective caesarean section: pragmatic randomised trial. BMJ. 2005. 331:662.
Article28). Stutchfield PR., Whitaker R., Gliddon AE., Hobson L., Kotecha S., Doull IJ. Behavioural, educational and respiratory outcomes of antenatal betamethasone for term caesarean section (ASTECS trial). Arch Dis Child Fetal Neonatal Ed. 2013. 98:F195–200.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Neonatal Respiratory Morbidities in Term Neonates
- Clinical Characteristics of Apnea in Full-Term Infants: Compared to Late Preterm Infants
- Low Birth Weight, Very Low Birth Weight Rates of Newborn Infants in Korea
- Preterm delivery between 34-36weeks of gestation; Is it danger?
- Observation of tooth mineralization of Korean neonates according to gestational age